During the COVID-19 pandemic, advanced clinical practitioners (ACPs) demonstrated their autonomy, transferrable skillset and high levels of expertise across the four pillars of advanced practice (Health Education England (HEE), 2017; Morley et al, 2022). Their responsiveness to change at a time when many traditional professional boundaries had dissolved was instrumental in not only in delivering patient-facing care, but also educating and preparing other staff in redeployment (Scott et al, 2022). Evidence suggests the acute impact of COVID-19 is under control due to successful strategies such as population prevention, education, vaccination and research (Chen et al, 2020; Coccia, 2021). However, an estimated 6.2% of the UK population self-identify as experiencing long Covid (LC) or post-Covid conditions, which raise complications in the management of the care of such individuals (Brown and O'Brien, 2021).
Background
LC comprises of symptomatic COVID-19 (which, by definition, is from 4 to 12 weeks after acute infection) and post-COVID-19 syndrome (which occurs from 12 weeks or more after acute infection) (National Institute for Health and Care Excellence (NICE), 2020). LC appears to be siloed by society, despite the detrimental impacts it has on a population health and healthcare professionals (Marshall-Andon et al, 2021; Rogers et al, 2022). The condition affects many organs, causing multidimensional clusters of symptoms of varying severity and durations that may unpredictably fluctuate (Brown and O'Brien, 2021); studies have suggested that individuals with LC may have a lower quality of life than those surviving cancer (Kuehn, 2021; Harada et al, 2022). The Office for National Statistics (ONS) (2022) estimates that 2 million people in England are experiencing LC symptoms 4 weeks post infection, with one in five facing a debilitating symptom impacting on their activities of daily living. Accuracy of this data may be contentious due to major challenges associated with a LC diagnosis and self-reported symptoms (Amin-Chowdhury and Ladhani, 2021). Wong and Weitzer (2021) identify that patients are often referred to LC clinics due to symptoms overlap, such as fatigue and dysautonomia, which are prevalent in both myalgic encephalomyelitis (ME) and LC. The absence of specific diagnostic criteria and a lack of adequate COVID-19 testing during the pandemic leaves a level of uncertainty among clinicians diagnosing LC (Ward et al, 2021). A lack of diagnostic tools to confirm LC, despite contemporary advancements in modern medicine, is challenging to comprehend. Therefore, effective and systematic history taking during clinical examination is crucial, as studies suggest that this will lead to 80.0% likelihood of an accurate diagnosis with appropriate differentials (Corrao and Argano, 2022).
Long Covid service delivery
NHS England and NHS Improvement (2021) have driven the development of a five-point progression LC plan, including a three-tier LC service model of self-management, primary care and MDT specialist teams within 90 integrated care systems. The promotion of self-management through the ‘Your COVID Recovery’ mobile application has been used by 11 million people to learn about the management of LC symptoms such as sleep, fatigue and anxiety; it is believed that 50.0% of patients can improve from this alone (Marshall-Andon et al, 2021). Lloyd-Evans et al (2022) states that this application has effectively reduced symptoms for people of all ages; however, it is indicated that patients' self-reported symptoms increase with time, which makes this data less conclusive. Despite low health technology literacy among older patients, the NHS continues to drive the implementation of health technologies (NHS, 2019). Evidence-based technology such as this requires promotion by ACPs, particularly since NHS England (2022a) identify that healthcare professionals account for 10% of people with LC.
Tier two of the LC model involves patients attending a GP practice for assessment. The GP's investigation aims to rule out differentials based on symptoms; if no alternative pathology is observed, only the GP can refer to LC services (NICE, 2020). Brennan et al (2022) found uncertainty of symptoms and pressures on GP workload as a cause for reduced LC service referrals. ACPs are well placed to support GPs in the assessment and identification of ‘red flag’ symptoms that require urgent action and referral (Greenhalgh et al, 2022).
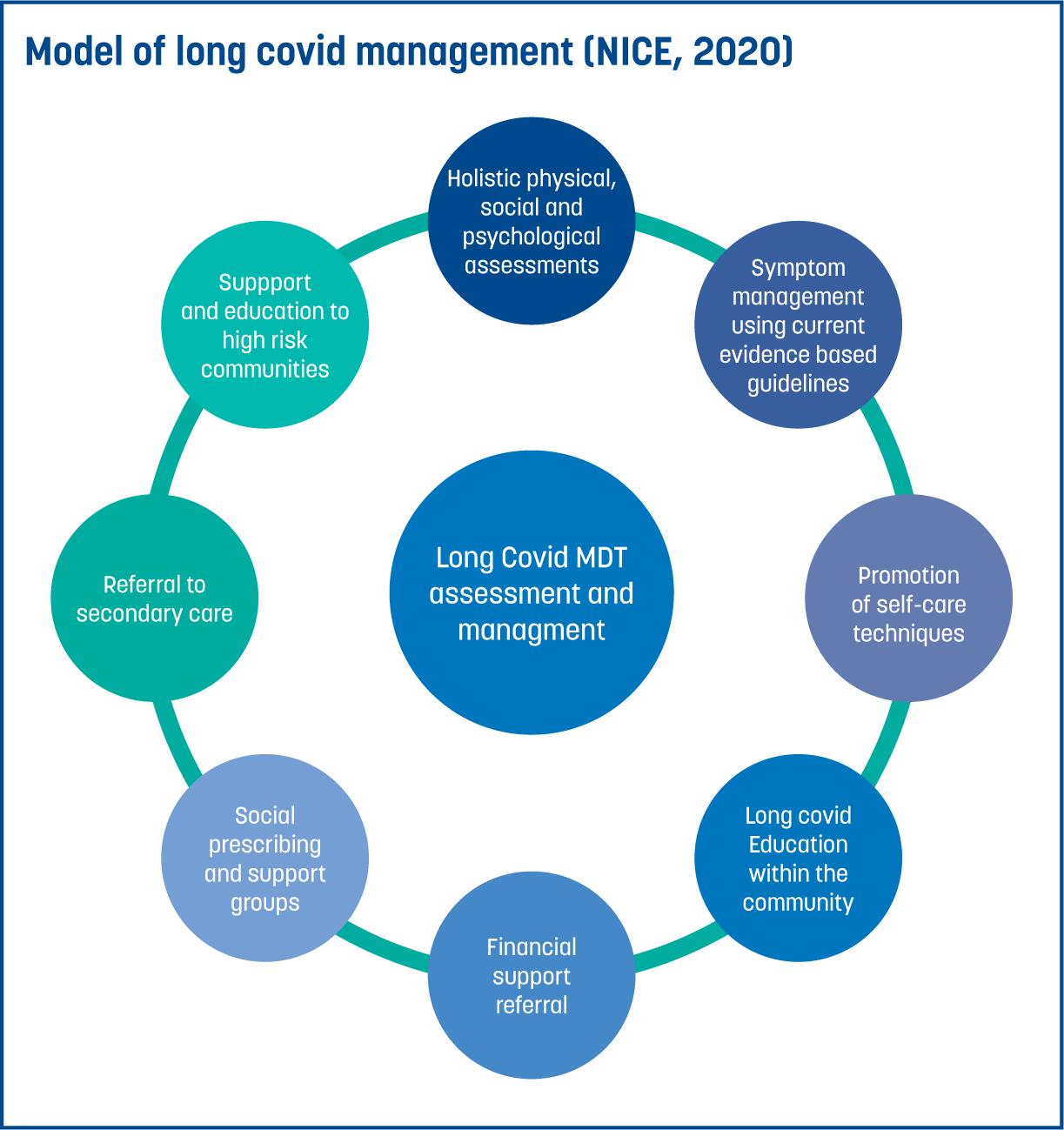
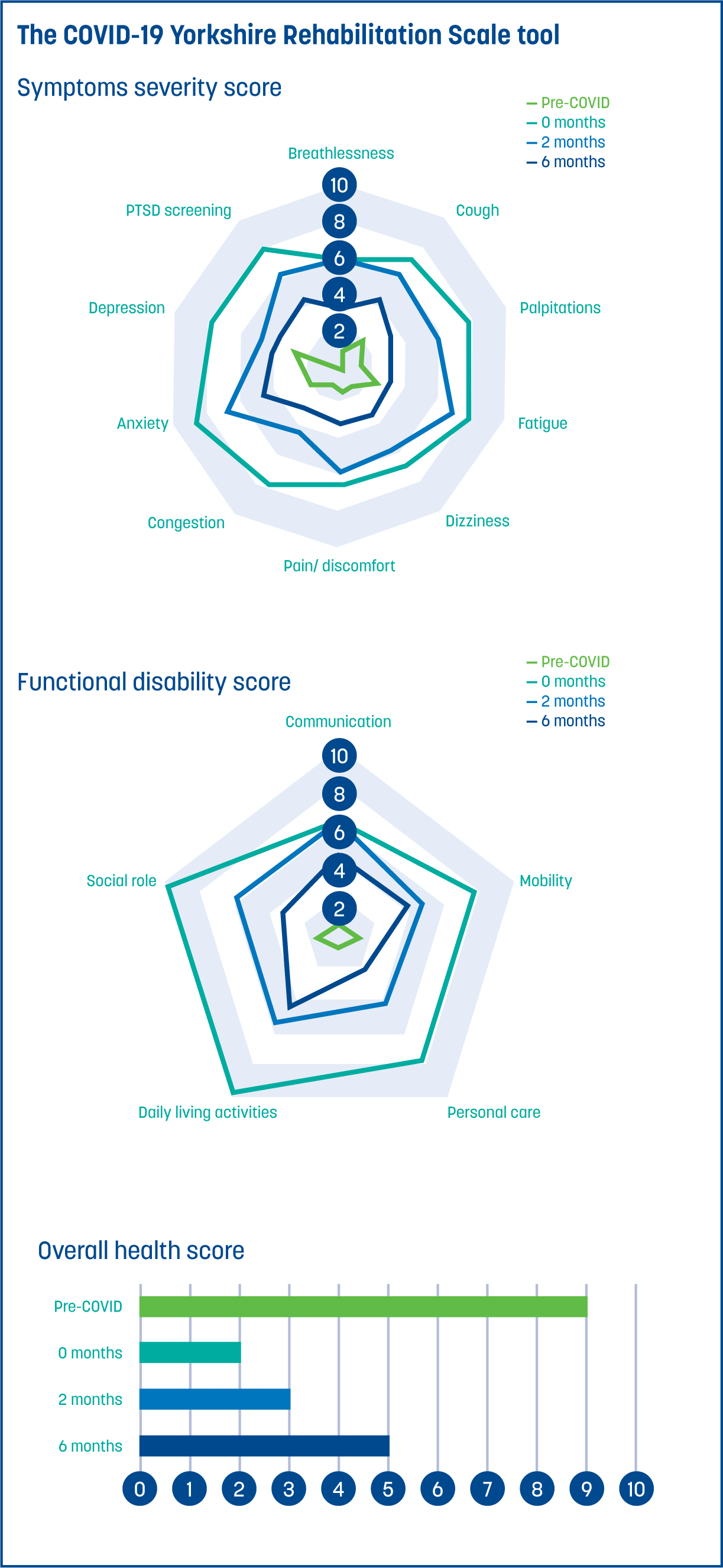
Furthermore, the World Health Organization (2021) reveals a lack of LC surveillance globally, particularly in European countries where LC services have been delayed. That being said, despite unsustainable NHS staffing, 90 LC services have developed into centralised research hubs to develop community education and provide rehabilitation pathways to improve patient outcomes through physical, social and psychiatric assessments (Parkin et al, 2021). The LC multi-disciplinary team integrates various professionals such as ACPs, doctors, therapists and psychologists to provide targeted individualised interventions using a specific set of outcome measures, such as the Borg rating of perceived exertion (NICE, 2020). Outcome measures, chosen based on patient-centred symptoms, are monitored at 8 weeks and 6 months post-initial admission onto the LC service (NICE, 2020); this can be a complex task due to the 203 symptoms associated with LC (Davis et al, 2021). The service adopts a model (Figure 1) of shared decision-making (NICE, 2020) to plan, rehabilitate and identify health needs through holistic assessment tools such as the COVID-19 Yorkshire Rehabilitation Scale tool (Figure 2), which has been proven to improve patient outcomes (Iacobucci, 2022; O'Connor et al, 2022). Tools are important to support decision making for ACPs in practice, but like other guidance, this depends upon the user's professional decision-making abilities and engagement with the individuals being assessed (Smyth and Mccabe, 2017).
Pathophysiology, diagnostics and management
Since the COVID-19 pandemic, £50 million of UK government funding has been invested into LC research projects (National Institute for Health and Care Research (NIHR), 2022). Viral persistence, organ damage, immune deregulation, autoimmunity, viral debris, reactivated virus and a disrupted microbiome are the main pathological causes of LC (Medinger and Altmann, 2022). For example, studies exploring gastrointestinal biopsies taken 4 months after acute COVID-19 uncovered live virus in a third of individuals, therefore suggesting an inflammatory response through cytokine storm leading to long term sequelae (Gaebler et al, 2021). LC is often reviewed in a comparable way to the Ebola or herpes virus, which also develops a chronic syndrome, harbouring reservoirs of the virus in human tissue months or years after initial infection (Proal and VanElzakker, 2021).
Neurological
Even though acute COVID-19 is predominantly a respiratory disorder, LC greatly impacts cardiovascular, immune and neurological systems (Medinger and Altmann, 2022). Brain scans on people with LC found decreased brain activity in the brainstem, cerebellum, the limbic regions and the olfactory nerve (Guedj et al, 2021). The neurological impact creates symptoms such as:
- Postural orthostatic tachycardia syndrome (PoTS)
- Brain fog
- Palpitations
- Dizziness
- Syncope
- Exercise intolerance (Dani et al, 2021).
LC creates an immune mediated disruption in the autonomic nervous system of patients with predisposed stress or genetic risk, which can result in hypotension, PoTS and vasovagal syncope (Medinger and Altmann, 2022). When a person stands, blood will accumulate in the lower limbs with gravity; as a result, baroreceptors in the heart detect reduced stroke volume and signal a release of adrenaline to increase volume back to the heart through tachycardia, which then subsides through homeostasis (Kavi, 2022). However, in orthostatic intolerance, the release of adrenaline causes palpitations, breathlessness and anxiety at higher levels, which can reverse this sympathetic response causing activation of the vagus nerve—resulting in syncope through hypotension. Unfortunately, these symptoms persist with LC, as the hypothalamus struggles to reach homeostasis, which creates debilitating cycles of fight versus flight for patients (Larsen et al, 2021).
Additionally, according to Public Health England (2017a), falls cost the NHS £4.4 billion a year and, as syncope is a common symptom of LC, this figure may increase. ACPs are pivotal facilitators in falls risk management, which is a key performance indicator of care driven by the NHS Long Term Plan (2019). LC symptoms of syncope and deconditioning during quarantine have increased falls in people aged over 65 years (Public Health England, 2021). ACPs responded to COVID-19 across different health and care contexts and continue to work across a variety of settings in day-to-day practice (HEE, 2020). By contemplating a patient's degree of frailty and the contribution of LC among other risk factors, ACPs could contribute to better outcomes and prevent harm across primary, secondary and tertiary disease prevention (Hoogendijk et al, 2019).
To diagnose PoTS-causing syncope, NICE (2020) guidelines identify the importance of a tilt table test; however, patient accounts identify the distress this test can have on exacerbating dysautonomic symptoms such as anxiety, palpitations and breathlessness. Therefore, as suggested by the NHS England (2022b) LC framework for nurses, understanding patient journeys and preferences is crucial for ACPs when informing personalised treatment plans and future service delivery. Although treatments are unavailable to reverse LC, symptomatic relief for PoTS is available through the prevention of hypovolaemia, low dose corticosteroids to reduce inflammation and beta blockers (Medinger and Altmann, 2022). While the focus remains on vagal nerve stimulation and the concept of neuroplasticity, which is the moldability of the brain through breathing exercises, this approach avoids exploring the exacerbating factors (Kavi, 2022). Despite the lack of quantitative evidence, Pilcher (2022), outlines the importance of practicing cold water swimming to reduce stress by developing a sense of autonomic control. ACPs could advocate self-care approaches by utilising social prescribing and support groups, which have the potential to reduce A&E attendances by 28.0% (Office for Health Improvement and Disparity, 2022).
The immune response: Mast Cell Activation Syndrome
Mast cells protect the body from pathogens and produce mediators that cause inflammation through the accumulation of histamine and cytokines (Medinger and Altmann, 2022). However, during LC, viral debris within the body is thought to reactivate mast cell development, resulting in high levels of mediators months to years after acute infection (Glynne et al, 2022). Despite the inconclusive sample size, 66.0% of patients reported that niacin supplements, low histamine diets and antihistamine medication alleviated these symptoms of headaches, seizures, fatigue and changes in allergy sensitivity, including anaphylaxis caused by LC (Afrin et al, 2020). Evidence suggests LC can increase the risk of allergies that must be identified to maintain caution and patient safety (Royal Pharmaceutical Society, 2021; Medinger and Altmann, 2022). This is crucial information for ACPs who prescribe. They must be cognisant of people from specific groups, such as older adults, children, women who are pregnant or breastfeeding, or have renal or hepatic impairment, in addition to LC, which requires consideration (Mitchell and Pearce, 2021).
The cardiovascular impact: micro-clots
Recent findings by Xie et al (2022) identified significant cardiovascular disease in the years after acute COVID-19 infection. This included arrythmias, myocarditis, heart failure and micro-clotting, in line with suggestions that LC viral debris attacks the endothelium causing organ damage, inflammation and imbalances in platelet formation (Castro et al, 2022). Despite the small sample size, researchers examined microscopic blood samples and discovered hyperactive platelet formation and hypercoagulation with fibrinolysis resistance (Kell et al, 2022). Micro-clots can inhibit oxygen exchange and cause shortness of breath, poor perfusion and anxiety, with evidence suggesting that anticoagulation therapy and statins could be used as treatment preventers (Patterson et al, 2021; Randeria et al, 2019). Consequently, cardiac-related issues caused by LC are suspected to increase demand and complexity for patients. ACPs will need to function collaboratively within proposed multi-specialist models of care to achieve the right balance between cost-effective investigations and sustainable service provision (Raman et al, 2022).
Mental health
Dennis et al's (2021) large-scale study identified on MRI imaging that 70.0% of younger participants had impairment of multiple organs 4 months after initial COVID-19 infection. The effects of LC are intensified by severe mental health outcomes, due to illness burden and damage to serotonin and dopamine levels (Attademo and Bernardini, 2021). Anxiety, depression, insomnia and post-traumatic stress disorder (PTSD) are among patient concerns; they have also reported feeling distressed about attending appointments and work, and spending days in bed without social interaction (Medinger and Altmann, 2022). This emphasises that LC can affect anyone and the seriousness of symptoms is not considered to be linked to the severity of acute infection (NICE, 2022). Davis et al's (2021) qualitative study examined patient experiences and the effect that LC has had on activities of daily living. Patients recalled feeling distanced from friends, family and employment, which resulted in feelings of isolation. Moreover, Bu et al (2021) identify that 45.0% percent of people talk to friends or family members to support their mental health through LC. This accentuates the value of ACP-patient communications and the underlying principles and consultation frameworks utilised within clinical practice, which are typically used to establish an accurate social and family history (Diamond-Fox, 2021).
Social determinants
Since the pandemic, The Kings Fund (2021) aimed to address the renewal of healthcare services. It set out five key priorities centred on creating an improved, fairer health system for the future. It highlighted the importance of identifying population health inequalities and advocating placed-based models of care (The Kings Fund, 2021). A safe and effective vaccination roll out during COVID-19 was essential and ACPs were part of the professional groups leading this approach (HEE, 2020). Nevertheless, the strategy for distribution has been, and remains, controversial, with many individuals and groups remaining vaccine hesitant (Wagner et al, 2022). Vaccine hesitancy is a multi-faceted issue made up of cultural, political and personal factors; however, evidence suggests prevalence is the highest among Black, Asian and minority ethnic communities, in part due to language barriers (Vergara et al, 2021). Additionally, 90.0% of poor health outcomes come from the wider social determinants of health, including social deprivation (Public Health England, 2017b). The ONS (2022) suggests that symptoms of LC are disproportionately impacting people in more socially deprived areas, signalled by a lack of GP attendances and inadequate public health education (Walker et al, 2021). ACPs can identify patient vulnerability and opportunities through tailored communication, translational services and information leaflets, as these interventions have shown to improve patient outcomes (Hunter et al, 2021).
The identified risk factors for LC are not exhaustive, however, contributors include de-conditioning caused by quarantine, stress, pre-existing long-term conditions, social deprivation and COVID-19 vaccination hesitancy (Sudre et al, 2021). While lockdown prevented acute COVID-19 mortalities, the impact of deconditioning during quarantine resulted in LC prevalence among athletes and the frail elderly; qualitative research highlights how returning to fitness can prove difficult due to exercise intolerance and induced dysautonomia (Lindsay et al, 2021). Metabolic diseases such as diabetes have also contributed to the risk of LC in studies, despite a lack of pathological understanding (Steenblock et al, 2022).
Not only does this indicate the need for ongoing research into pathology, but it also highlights the impact that restrictions, chronic conditions and social determinants can have on LC prevalence. Such developments echo the ACPs commitment to appraising the developing evidence base, which is integral to the core pillars of practice (HEE, 2017).
Conclusion
LC appears to be a siloed, complex topic with a lack of reversible treatment options, despite the vast research and global funding. The research reviewed within this paper recognises some key areas for development for the ACP role, such as managing falls associated with LC dysautonomia and understanding the complexities of care for those with existing chronic diseases (such as cardiovascular and metabolic disease).
Further considerations for prescribers, such as atopy and increased susceptibility for mental health conditions, reflects the continued growth of knowledge within the field. Acknowledging the contribution of the social determinants of health in LC can play a vital role in the identification and promotion of LC strategies to ensure improved patient outcomes.
More research into the identification of LC patients may facilitate referrals to appropriate services and support ACPs in the decision-making process from the beginning.
While the ACP role offers a vehicle through which those requiring the effective management of LC and other co-morbidities can be supported, it has come under increased demand due to winter pressures, inadequate staff retention and the cost-of-living crisis. Additional funding and a greater allocation of resources is required to ensure that the ACP role is able to meet future demand in relation to LC treatment plans.
KEY POINTS
- A total of 2 million people in England are experiencing long Covid (LC) symptoms, with one in five facing debilitating symptoms
- LC is a multi-organ chronic condition caused by viral persistence, organ damage, immune deregulation and disrupted microbiome
- LC impacts cardiovascular, immune and neurological system, which can contribute to falls, micro-clots and allergy risks
- LC risk factors are quarantine-induced de-conditioning, stress, pre-existing long-term conditions, social deprivation and COVID-19 vaccination hesitancy.
CPD / Reflective Questions
- What could be done to enhance long Covid (LC) patient assessments in your clinical setting?
- What current evidence-based tools are you aware of to support a LC diagnosis?
- Using knowledge gained from this article and further study, write a revalidation reflection on the management of LC.


