This case study will introduce, evaluate and critically analyse the case of a female patient, aged 80 years, who was seen in a secondary care setting following surgery for an intracapsular fractured neck of femur. The perspective is that of a trainee advanced clinical practitioner (tACP) working under full supervision, and the case study is written as part of the academic requirements for the course, presenting the practitioner as an independent prescriber.
The patient had fallen from a standing height at home, a couple of days prior to presentation, sustaining an intra-capsular fracture of the neck of femur, thus fulfilling the definition of a fragility fracture (National Institute for Health and Care Excellence (NICE), 2017; International Osteoporosis Foundation (IOF), 2024). She had undergone internal fixation of the fracture with a hemiarthroplasty prosthesis under the care of the orthopaedic surgeons.
As per NICE guidelines (2023a), the employing NHS trust of the tACP has an integrated orthogeriatric service, with which the student was on placement at the time. In the UK, orthogeriatric co-management has been in place since the 1960s (Folbert et al, 2017). Provision should be offered from the time of admission (NICE, 2023a), with the focus being the optimisation of the patient prior to surgery (Pioli et al, 2018), followed by ongoing intervention, which includes multi-disciplinary team review (NICE, 2023a). It is recognised that the initial occurrence of a fragility fracture is the most significant risk factor for a subsequent fracture, and that mortality following a second hip fracture can be 50% higher (Piolo et al, 2018). Despite this, anti-osteoporosis medication has been seen to be poorly utilised following hip fracture; thus, orthogeriatric clinicians should aim to have the confidence to commence treatment in the acute setting (Pioli et al, 2018; NICE, 2021).
Setting
The student prescriber in this case is a chartered physiotherapist and, as such, is governed by the code of conduct of the Health and Care Professions Council (HCPC) (2016). The Chartered Society of Physiotherapy (CSP) (2018) has also produced a practice guidance document for independent and supplementary prescribers that sets out the required skills and educational attainment of their members who wish to be prescribers. Additionally, this document offers clear guidance on the required skills for managing patient assessment, and outlines the need for patient involvement in prescribing decisions. The latter element is of the utmost importance in this case study.
The HCPC Standards for Prescribing (2019) set out the principles for education providers alongside prescribers. The HCPC has adopted the Royal Pharmaceutical Society (RPS) (2021) Competency Framework for all prescribers, which will provide a structured backdrop to this case study, as it is based on the Patient Consultation Competencies 1–6.
Non-medical prescribing has become an established part of advanced clinical practice in the UK, driven by the need to provide support in the context of the increasing complexity of patient care and mitigate the demand on the NHS (Mitchell and Pearce, 2021; Graham-Clarke et al, 2022). Research comparing outcomes for patients seen by prescribing and non-prescribing physiotherapists has reported high levels of patient satisfaction and improvements in quality of life for those patients seen by prescribers (Carey et al, 2020). An unfavourable finding of this same study, however, was related to the cost implications of utilising prescribers in this way, due to longer consultations and the amount of time spent discussing prescribing decisions with medical colleagues (Carey et al, 2020).
Competency 1: assess the patient
The purpose of the patient consultation in this case study was: 1) to assess the risk of further fractures, based on bone health parameters and level of falls risk; and 2) to evaluate the appropriateness of oral bisphosphonate therapy, specifically alendronic acid. The first competency of the RPS Framework (2021) covers the need to assess the patient and offers clear guidance in achieving clinical effectiveness and safety during this phase.
On reviewing the literature, it can be seen there is a wealth of documentation examining models of patient consultation; however, these have predominantly been created for medical practitioners (Denness, 2013). Senior (2021) observed that, with experience, a clinician is likely to combine elements of more than one model to achieve the most favourable outcome for an individual patient. For this case study, the format used was the Calgary–Cambridge model (Kurtz and Silverman, 1996), which has been shown to be an accepted framework and one that is used frequently by prescribers (Mitchell and Pearce, 2021).
The two main principles underlying this model comprise building a relationship with the patient and structuring the consultation while following the five stages of the model (Munson and Wilcox, 2007). Manalastas et al (2021) developed a system for visualising consultation structure and noted that, if well-organised, a consultation can work to encourage patients to be actively involved in the management of their health. The Calgary–Cambridge model recognises the concerns of the individual and prompts patient involvement in decision-making (Munson and Wilcox, 2007). This is highly relevant, as it has been found that adherence to alendronic acid can be poor: as low as 50% at 12 months due to a variety of factors, including side effects and the strict method for administration (NICE, 2017; Compston, 2020; IOF, 2024). It has also been noted that treatment success is determined by adherence to the regime (NICE, 2017; McCloskey et al, 2018). Adherence has been defined as the extent to which a patient's actions are in line with the agreed recommendation (NICE, 2009).
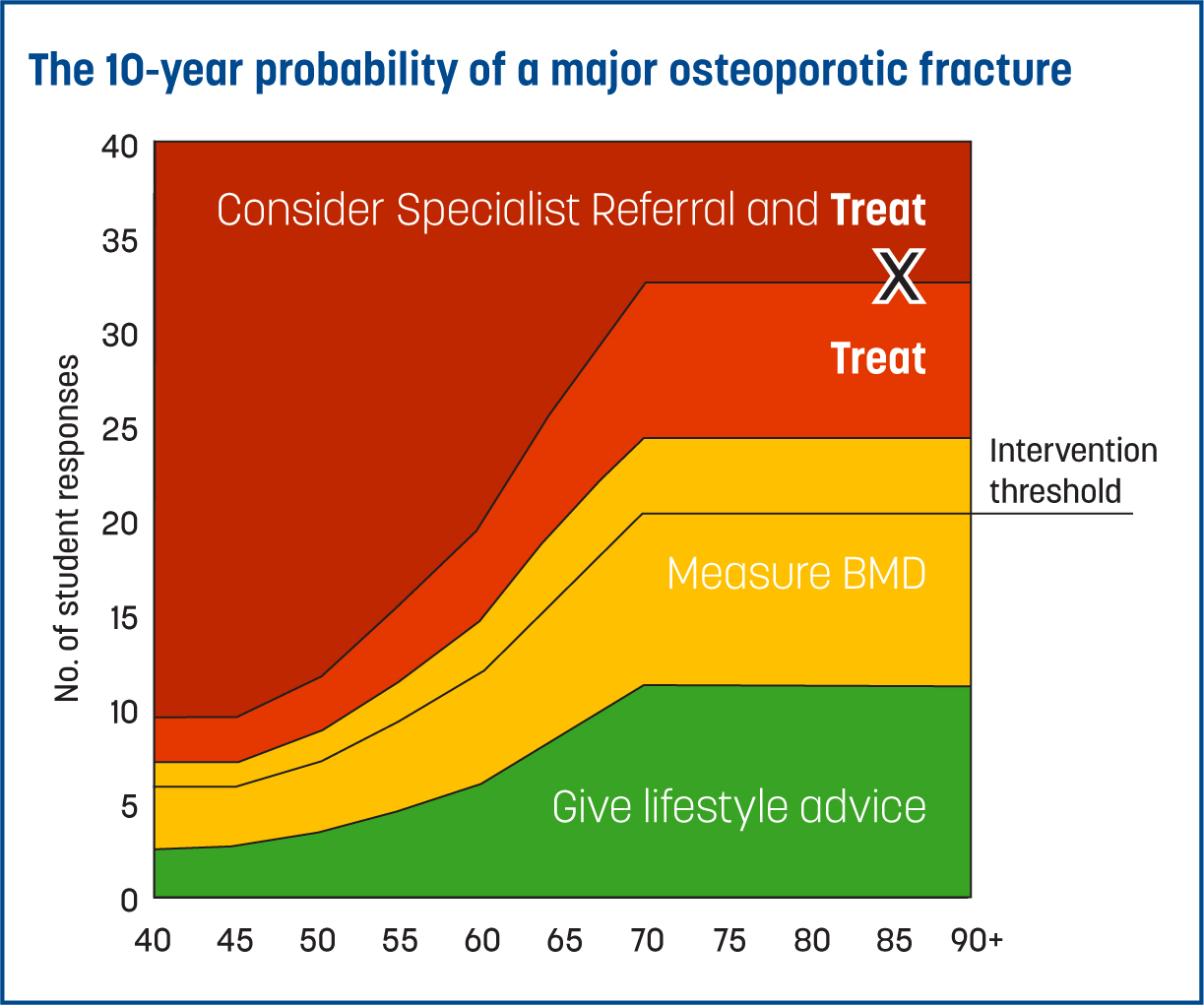
As this case study's patient had sustained the femoral fracture after falling from a standing height while in the kitchen, the injury is termed a fragility fracture. It was thus appropriate to consider a diagnosis of osteoporosis. This is a disease characterised by low bone mass and a gradual deterioration of bone structure, which leads to an increase in vulnerability to fracture; osteoporosis can be symptomless until fracture occurs (LeBoff et al, 2022). NICE guidelines (2012) recommend assessment of fracture risk in all patients with a previous fragility fracture. The employing NHS organisation of the tACP utilises the Fracture Risk Assessment Tool (FRAX) score as a tool for establishing the risk of fragility fracture and identifying those patients that will benefit from preventative treatment (Kanis et al, 2018). FRAX is a computer-based algorithm that uses independent clinical risk factors alongside bone mineral density (BMD) measurements, where available, to calculate the 10-year probability of sustaining a major osteoporotic fracture (Parsons et al, 2020). BMD measurement alone has been shown to have very low sensitivity for fracture risk prediction (Shepstone et al, 2018) and, as such, is inadequate when not used in combination with assessment of risk factors (McCloskey et al, 2018; Compston, 2020). Thus, an imperative part of the history-taking process was to establish the presence or absence of clinical risk factors—such as family history, smoking and alcohol use and relevant comorbidities—to allow completion and interpretation of the FRAX score. In this case study, the calculated FRAX score showed that the 10-year risk of major osteoporotic fracture was 32% and that of hip fracture was 20%. This exceeded the threshold for treatment (Figure 1), even without BMD measurements; therefore, consideration of bisphosphonate therapy was appropriate (National Osteoporosis Guidance Group (NOGG), 2021).
Commencement of treatment should not be delayed in this type of patient while awaiting BMD measurements (NICE, 2017; Conley et al, 2020). A consultation regarding bone health and fracture risk should include assessment of diet, physical activity levels, lifestyle and falls risk factors, along with the consideration of pharmacological treatment options (LeBoff et al, 2022). Physiological assessment parameters should include full blood count, renal function, serum albumin and bone profile, along with liver function tests, vitamin D, parathyroid hormone, and thyroid-stimulating hormone levels (NICE, 2017; LeBoff et al, 2022).
While these tests were all conducted, it is beyond the scope of this case study to describe the findings in detail. Critically, the patient's creatinine clearance was calculated at 49 mL/min, which is adequate for the pharmacokinetics of alendronic acid (Joint Formulary Committee, 2022). Furthermore, the patient was found to be vitamin D replete but hypocalcaemic, thus requiring correction of serum calcium levels prior to commencement of alendronic acid (NOGG, 2021). In the first instance, Adcal-D3 was prescribed, with a daily dose of 1.5 mg/400 iu (Joint Formulary Committee, 2022); the patient was advised to maintain a daily dietary intake of calcium of at least 700 mg (NICE, 2023b).
Thorough assessment of the patient's past medical history and allergies also allowed the student to identify any specific risk factors for the development of adverse effects to alendronic acid—for example, dysphagia or upper gastrointestinal disorders (Zullo et al, 2019; Joint Formulary Committee, 2022). These were satisfactorily ruled out.
Competency 2: identify evidence-based treatment options available for clinical decision-making
This competency covers the identification of evidence-based treatment options and consideration of both pharmacological and non-pharmacological treatment (RPS, 2021). With regards to the management of osteoporosis, advice on lifestyle modifications is paramount (Conley et al, 2020; NOGG, 2021; Brook-Wavell et al, 2022; NICE, 2023b). Waltman et al (2022) details these measures as maintaining adequate calcium and vitamin D intake; smoking cessation; weight bearing and resistance exercise; and falls prevention measures. In addition, it is reported that chronic alcohol use, malnutrition and obesity are factors that increase the risk of osteoporotic fractures (Tachiki et al, 2019). There is evidence linking physical activity levels with bone health, and it has been shown that regular exercisers have a lower incidence of fractures (Brook-Wavell et al, 2022). Importantly, Brook-Wavell et al (2022) also highlight that appropriate exercise reduces the risk of falls and thus further lessens the risk of fractures. Accordingly, the decision to prescribe alendronic acid for this patient was made, alongside the conducting of a robust review of their modifiable risk factors and clear advice given on strategies to reduce the risk of further fractures.
As the patient had full mental capacity (Nicholson et al, 2008), the risks and benefits of alendronic acid were discussed with them to provide a good understanding of possible adverse effects—namely, gastrointestinal disorders, joint or muscle pain and the risk of atypical femoral fractures (Compston, 2020; Joint Formulary Committee, 2022). As the name implies, atypical femoral fractures are a rare adverse effect of bisphosphonate therapy; as such, it has been stated that the risk of such a fracture is outweighed by the obvious benefits from overall reduction in osteoporotic fracture risk (Black et al, 2022). In addition, it was necessary to discuss the patient's dental health and to ensure any required dental surgery was undertaken prior to commencement of treatment, to reduce the risk of developing the rare side effect of osteonecrosis of the jaw (Conley et al, 2020; NICE, 2023b). Time was also spent ensuring that the patient was aware that alendronic acid is effective at improving BMD and preventing fractures (Compston, 2020; Dong et al, 2021; Black et al, 2022) and discussing the risk of further fractures if treatment was not commenced (Conley et al, 2020).
Alendronic acid is a drug that falls under the bisphosphonate group of medicines, which were first described as early as the 1960s, meaning that there has been extensive associated research conducted over many years and a subsequent good understanding of the pharmacology of these drugs developed (Cremers et al, 2019). Alendronic acid works by binding to the inorganic mineral crystals in bone tissue, known as hydroxyapatite, and acting to inhibit osteoclast-mediated bone resorption (DrugBank, 2023). It binds especially well at active sites of resorption and in trabecular bone, resulting in non-homogenous skeletal distribution (Cremers et al, 2019). Where it binds in the bone tissue, it is distributed due to acidification of the area and moves into the osteoclasts by endocytosis, inducing cell apoptosis and thus inhibition of osteoclast activity (DrugBank, 2023). Alendronic acid will then either be released for excretion or will be covered in newly formed bone and released later (Cremers et al, 2019). Notably, bone formation pathways are unaffected, and new bone formed during treatment with alendronic acid will be of normal quality (Electronic Medicines Compendium (EMC), 2022).
Understanding the pharmacokinetics of alendronic acid has led to identification of optimal therapeutic regimens (Dong et al, 2021). Alendronic acid is absorbed in the stomach, duodenum and ileum but is poorly absorbed, with a bioavailability of only 0.64% in women (EMC, 2022), which can be further reduced if taken with food, drinks or calcium supplements (Cremers et al, 2019). It is rapidly distributed to bone tissue or is excreted in the urine. Alendronic acid does not undergo any biotransformation and is eliminated, unchanged, via glomerular filtration at the kidneys and excreted exclusively in urine (EMC, 2022). In the presence of renal impairment, alendronic acid will accumulate and is not suitable for patients with a creatinine clearance of less than 35 mL/min (Joint Formulary Committee, 2022). Risendronate is a suitable alternative for these patients and can be used where the creatinine clearance is equal to or more than 30 mL/min (Joint Formulary Committee, 2022). The terminal half-life of alendronic acid is around 10 years, reflecting its slow release from the skeleton; indeed, bisphosphonates have been found in urine years after cessation of the drug (Cremers et al, 2019).
On reviewing the literature with regards to the use of alendronic acid, some consistent themes emerge. Firstly, it is clearly effective at reducing the risk of fractures and at increasing BMD when used in conjunction with adequate dietary or supplementary intake of calcium and vitamin D (van Geel et al, 2018; Zullo et al, 2019; Black et al, 2022). Secondly, it is evident that there is no benefit in prolonging treatment with alendronic acid beyond 5 years; at this point, patients should be risk assessed and considered for a ‘drug holiday’ (Villa et al, 2016; NOGG, 2021). Dong et al (2021) conducted a systematic review and network meta-analysis reviewing 14 randomised controlled trials with 11450 participants. The authors of this substantial review were able to show that alendronic acid produced significant increases in BMD at the femoral neck and lumbar spine and that, for every decrease of 1 of the standard deviation in the BMD, there was a 2–3-fold increase in fracture risk (Dong et al, 2021). Black et al (2022) conducted a large cohort study encompassing 196129 women and concluded that, if 10 000 women are treated with bisphosphonates for 3 years, around 1000 fractures will be prevented. These same authors were also able to demonstrate that, after cessation of bisphosphonates, the fracture-reducing effect was retained for 5 years (Black et al, 2022). The NOG Guidelines (2021) are clear: in patients for whom treatment is indicated, bisphosphonates should be offered; where the patient has experienced a fragility fracture, as in this case, treatment should be started without delay, as the risk of further fracture is highest immediately after the first fracture.
Competency 3: present options and reach a shared decision
This element was conducted over two separate sessions, to ensure that the patient understood the risks and benefits of treatment with alendronic acid, and included a robust conversation about possible side effects and how to recognise them (Parsons et al, 2020). An alternative bisphosphonate is zoledronic acid, which can be given annually via intravenous infusion and has been shown to not only give greater gains in BMD (Compston, 2020), but also displays higher rates of adherence (Bastounis et al, 2022). Indeed, the NOG Guidelines (2021), as also recommended in the NICE Guidelines (NICE, 2023b), state that zoledronic acid should be offered as first-line treatment following hip fracture.
Competency 4: prescribe
The fourth RPS competency covers the prescribing of the medicine (RPS, 2021). Thus, alendronic acid was prescribed, as per the Joint Formulary Committee (2022), as a 70 mg tablet weekly, with the patient to start treatment once home from hospital. This is in line with the trust's protocol of commencing bisphosphonate therapy 14 days post-operatively for patients following fractured neck of femur. It has been found that adherence is improved if alendronic acid is prescribed at 70 mg weekly instead of 10mg daily (Bastounis et al, 2022). The duration of treatment is 5 years, followed by a ‘drug holiday’. As per the Joint Formulary Committee (2022), alendronic acid should be taken on an empty stomach with a large glass of water while sitting upright or standing, and at least 30 minutes before food, drink or other medicines.
Competency 5: provide information
Due to the importance of this information, written materials were provided to the patient in order to minimise the risk of adverse effects and optimise adherence, as per Competency 5 of the RPS Framework (2021). It is important to assess the health literacy of each patient and present the information in the most appropriate style, as unmet needs regarding prescribing information can have significant consequences and lead to poor treatment adherence (Raybould et al, 2018). Lopez-Olivo et al (2021) evaluated online resources for patients with osteoporosis and found that, if the information is evidence-based and unbiased, it could help patients with their lifestyle choices, in their decision making and with the correct use of medications. On reflection, directing the patient of this case study to high-quality online resources could have empowered her further in managing her own condition. The final element of information provision to the patient was the safety-net advice, ensuring the patient was aware of potential adverse effects of alendronic acid and the action to take in the event of developing specific symptoms (Compston, 2020). The patient was also made aware of the Yellow Card Scheme operated by the Medicines and Healthcare products Regulatory Authority, and how to report an adverse drug reaction (Joint Formulary Committee, 2022).
Competency 6: monitor and review
As this consultation took place in a secondary care setting, clear communication with the patient's GP was essential (Gai et al, 2020). Relating specifically to the prescribing decisions made, the hospital discharge letter was used to request that the general practitioner monitor calcium and vitamin D levels and offer supplementation if required in the future, as well as to continue to prescribe alendronic acid at the same dose for 5 years if tolerated by the patient. The GP was also asked to refer for a bone density scan, to facilitate the addition of BMD measurements to the patient's FRAX score when reassessing fracture risk in the future (NICE, 2017; NOGG, 2021).
Conclusions
In summary, this case study has discussed a patient, aged 80 years, who was prescribed alendronic acid. The dose selected was as per the Joint Formulary Committee (2022) as treatment for postmenopausal osteoporosis; the duration of treatment was to be 5 years, with the patient's GP responsible for monitoring and review of this medication.
The consultation called upon a range of communication skills to ensure that the patient understood the treatment options and the risks and benefits of treatment. By taking the time to meet with the patient on two occasions, it was felt that the information had been well understood and retained, and there could be a good level of confidence regarding future treatment adherence (NOGG, 2021). Providing access to multi-media information sources could have enhanced this process further (Lopez-Olivo et al, 2021), and identification of appropriate sources would be a highly valuable service development. This case study illustrates the importance of a multifaceted approach in osteoporosis management that must be personalised to each patient.


