Medical staff shortages and the UK's ageing population have resulted in the NHS seeking alternate models of healthcare (NHS England, 2014; NHS, 2019). Utilising pre-existing qualified healthcare staff, who have undergone advanced training, is one method of enhancing capacity, productivity and efficiency (NHS, 2019; Health Education England, 2022). One such example is advanced nurse practitioners, who have been successfully employed in healthcare in formal advanced roles since the early 1990s (Leary and MacLaine, 2019). Advanced clinical practice has expanded in the last decade, and now includes allied health professionals (AHPs), such as physiotherapists (Leary and MacLaine, 2019; Timmons et al, 2023). With the acquisition of advanced skills, AHPs have been recognised as an untapped workforce resource that can assist with transforming services (NHS England, 2017; NHS England, 2022).
Background
Community hospitals, which support inpatients that require less acute intervention but are unable to return home safely (Gladman et al, 2017), face unprecedented demand and strain (NHS Digital, 2021; NHS Digital, 2022). Thus, employers have sought alternate models to support the delivery of care in this setting and have recruited physiotherapy ACPs to work as part of the inpatient medical teams, alongside nurse ACPs and doctors. While well established in advanced practice roles such as first contact practitioners (Mercer and Hensman-Crook, 2022), physiotherapists working as ACPs in inpatient medical teams is a new evolution of the profession. As research on staff experience of ACPs working in inpatient settings is limited to the nursing profession (Dalton, 2013; Cowley et al, 2016; Halliday et al, 2018; Batty, 2021), it is currently unknown how ward staff would experience and respond to working with different professions, such physiotherapists, in this advanced role.
Aim
This research study aimed to explore the experience of ward staff working with physiotherapy ACPs in the inpatient medical team in a community hospital setting.
Methods
Ethical considerations
Ethical approval was obtained from the local university and the employing NHS trust in November 2022. A written confirmation letter was signed by the local university and employing NHS trust.
Sampling and selection strategy
A purposive sampling strategy was used to recruit 16 participants, who had been deemed suitable to provide detailed information on their experiences (Whitehead and Whitehead, 2016). The sample included: doctors, nurse ACPs, staff nurses, ward managers, physiotherapists, occupational therapists and pharmacists. Their suitability had been determined by them having consistently worked closely with the physiotherapy ACPs. Participants were identified from the ward rotas and were invited via email. They were provided with a participant information sheet that explained the purpose of the study. Written informed consent was obtained. All participants had worked with the physiotherapy ACPs for at least 6 months.
Data collection
The data were collected from three community hospitals operated by a large NHS Trust located in the West Midlands, UK. The physiotherapy ACPs in the team had varied clinical backgrounds and were all within their final year of their MSc in advanced clinical practice at the time of the study. An interview-based questionnaire was used to gather the data. A total of 16 completed interview-based questionnaires were received and analysed.
Data analysis
Data from the interview-based questionnaires were analysed using the Braun and Clarke thematic analysis model (Braun and Clarke, 2006); the model is well-recognised as robust and reliable (Byrne, 2022). Data extracts from the interview-based questionnaires were used to identify both the themes and subthemes, and to demonstrate the credibility of the findings.
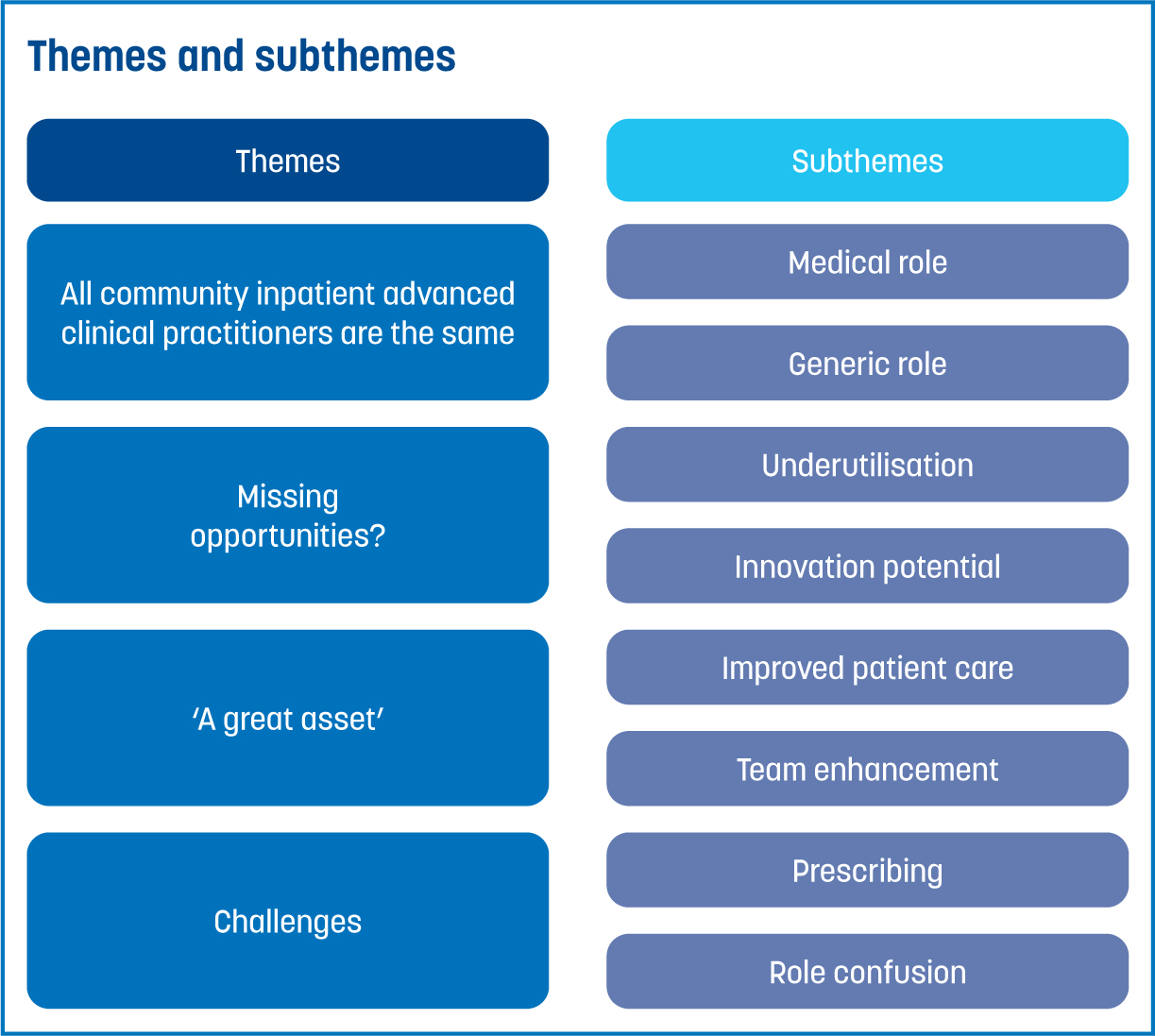
There were four themes identified from the data (Figure 1):
Findings
The themes and subthemes presented in these findings highlight both the current opportunities and challenges facing physiotherapy ACPs.
All inpatient advanced clinical practitioners are the same
This theme consisted of two subthemes: medical role and generic role.
Medical role
Some ward staff viewed physiotherapy ACPs as undertaking a medical role due to the type of care and support they provided to patients:
‘As with all the other medics/nurse ACPs, they provide medical care for patients and are available to answer questions from staff, patients and relatives about the patients care from a medical point of view’
One doctor detailed how the physiotherapy ACPs had a role in providing the medical continuity to patients from admission through to discharge:
‘They are part of the medical team and undertake medical assessment, medical management, rehab facilitation and discharge’
Generic role
Other ward staff felt that the physiotherapy ACPs did a generic role, or no different to that of another ACP:
‘The role is generic, with ACPs providing a weekday service that includes assessing new admissions to community hospitals, planning care and carrying out medication reviews’
The generic nature of the role was also highlighted by members of the wider ward multi-disciplinarily team (MDT):
‘The physio ACP role is the same as the nurse ACP role’
However, there was concern that such a generic role could result in the loss of the working identity of the physiotherapy ACPs:
‘There may be a risk of losing their professional identity’
Missing opportunities?
This theme consisted of two subthemes: underutilisation and innovation potential.
Underutilisation
The ward staff were clear that the ACP physiotherapists' full potential was not being used due to the limited use of their background skills and knowledge:
‘Physiotherapist ACPs should be given the opportunity to use their physiotherapy skills to provide more patient-focussed care and clinical continuity. They could help to further bridge the gap between doctors and therapists, improving understanding and communication between teams which ultimately would benefit patients’
The ward physiotherapists also shared a similar view:
‘If being used correctly, they could be utilised to bring their physiotherapy skills into the medical team and be advocates for the transfer of highly specialised physiotherapy skills into the medical environment’
Innovation potential
Ward staff also recognised the innovation potential that ACP physiotherapists could have on improving patient care, if utilised correctly:
‘The potential is huge, but currently not utilised. I personally find this frustrating … physio ACPs aren't nurse ACPs. They should be leading the AHPs’
This view was shared by nurse ACPs:
‘I believe there are developments yet to be made that focus on the advancement of the particular professional role of the ACP utilising their specific skills set, rather than solely providing a generic ACP service entirely based upon meeting medical need’
A great asset
This theme consisted of two subthemes: improved patient care and team enhancement.
Improved patient care
The professional background skills and knowledge of physiotherapy ACPs were recognised as valuable:
‘Their expertise in respiratory management, musculoskeletal and neuro conditions is invaluable, as well as the knowledge of helping and supporting patients and their families with living with frailty’
‘The advantage of the ACP with [a] physio background is that they understand the physical issues involved with patients’
The ward therapists also believed that the physiotherapy ACPs improved patient care and positively impacted on safer patient discharges:
‘They can link current medical presentation and potential for change in health, to consider the most sustainable discharge plans’
In contrast, the ward pharmacist highlighted the physiotherapy ACPs' alternative views on patient care:
‘Different clinical approach. They will instinctively assess/review a patient differently to other clinical groups. This doesn't mean they don't cover everything, they just review things differently’
Team enhancement
The physiotherapy ACPs brought a different perspective to their team, influencing a change in the clinical practice of others:
‘They pull the team together…it has made the other members of the ACP team broaden their thinking when it comes to managing frail elderly patients. Thinking about non-pharmacological options and other support mechanisms that could be used to enable safe discharges’
The wider MDT also experienced the value physiotherapy ACPs brought to the wider team:
‘I can honestly say that the physio ACP has been a great asset to the team and their background has enhanced the team. They bring their own individual knowledge in a different area’
The physiotherapy ACPs were viewed as advocates for the importance of therapy and rehabilitation:
‘Being advocates from a rehabilitation perspective and physiotherapy perspective within the medical team’
They were also perceived to bridge a gap between teams, which was experienced by both those in the inpatient medical team and the ward therapists:
‘Their expertise as physios enables a bridging of the gap within the community hospital between the medical team and the therapy team, which really can enhance overall care’
Challenges
This theme consisted of two subthemes: prescribing and role confusion.
Prescribing
Prescribing was a challenge for the physiotherapy ACPs because of the profession's legal restrictions. This limited the physiotherapists' ability to fully undertake the inpatient ACP role, when compared to the nurse ACPs and medics in the team. This was reflected in the feedback from their colleagues:
‘The only disadvantage is the lack of professional recognition to be able to prescribe the full range of medications. I feel this takes away some of the credibility they bring to the team and makes the ACP physio feel they are lacking in their ability to be able to practice to the full remit of an ACP’
These prescribing restrictions were also recognised by the wider MDT:
‘Their governing body restricts their prescribing. This has caused issues within community hospitals, mainly due to a lack of understanding of others, not the physiotherapy ACPs’
Role confusion
Ward staff recognised that the physiotherapy ACP role lacked a clear range of duties, which caused confusion among the therapists:
‘Not a clearly defined scope of practice, so from a therapy perspective it is sometimes unclear which elements of patient care is appropriate to approach the physiotherapy ACP with’
‘I feel like more knowledge given to staff on the role of the physiotherapy ACP would be helpful’
Discussion
This is the first study to contribute new knowledge on the experience of ward staff of working with physiotherapy ACPs as part of an inpatient medical team in a community hospital setting.
Professional erosion
Some ward staff stated that physiotherapist ACPs provided only general medical care to patients. This resulted in some ward staff feeling that all community inpatient ACPs were the same, regardless of their professional background. This sentiment suggests that the individual value that each different profession can bring to the ACP role has been lost.
This perception may reinforce the view that inpatient ACPs are substitutes for doctors; this can leave ACPs in a vulnerable position, being expected to perform to the same standard without having received the same extensive medical training or remuneration. This has been seen widely in other practice settings (Jones et al, 2015; Cowley et al, 2016; Goldberg, 2016; Halliday et al, 2018; Batty, 2021; Evans et al, 2021) and is the consequence of ACPs being ‘used’ in a rigid way in a medical model of care.
Stakeholders, especially employers, should recognise that ACPs can only enhance and transform services and patient care if their individual professional differences, skills and knowledge are used (NHS, 2019; Evans et al, 2020; NHS England, 2020). Furthermore, the use of ACPs in generic roles can cause the erosion of professional specific skills and knowledge, resulting in the loss of a strong professional identity associated with a core profession (Hooks and Walker, 2020). As ACPs are yet to be recognised as a professional group in their own right (Anderson et al, 2020; Lawler et al, 2022; Timmons et al, 2023), professional isolation and the lack of role acceptance by colleagues are significant risks for individuals working in generic roles where there is little affinity to their background profession.
Generalist or specialist?
Ward staff strongly felt that physiotherapy ACPs were not being used to their full potential. As the physiotherapy ACPs were being used to complete generalist tasks, they had limited opportunities to fully use their specific skills and knowledge. For example, some physiotherapist ACPs were restricted in their capacity to address the complexities encountered in therapy, due to their commitment to day-to-day medical tasks. Generalist ACP roles place ACPs at risk of the loss of core profession-specific competencies (Hooks and Walker, 2020). While some ward staff felt the physiotherapy ACPs were suited to this generalist role, others felt that the functionality needed to be a more specialist, profession-specific advanced role.
This specialist versus generalist debate between ward staff in this study mirrors findings from Timmons et al (2023). Using ACPs in specialist roles is not unreasonable; the NHS People Plan (NHS, 2020) highlights that multi-professional teams are expected to be the future of the NHS workforce, and that these teams should build on the full range of experience/capabilities of different professional backgrounds, including those working as ACPs.
However, employers seem to have been using ACP roles in a generalist way to directly substitute for doctors and fill staffing shortfalls (Hooks and Walker, 2020; Evans et al, 2021; Thompson and McNamara, 2022). This approach incurs several problems, specifically: perpetuating the notion of role substitution; and making it more difficult to establish the ACP role in its own right and profession (Thompson and McNamara, 2022). Collectively, these factors can potentially lead to ACP role dissonance, as ACPs may find themselves unmotivated by not working at the advanced practice level they have aspired to (Hooks and Walker, 2020; Steward-Lord et al, 2020; Taylor et al, 2022).
Variable prescribing rights
Prescribing was a widely acknowledged as a challenge for the physiotherapy ACPs working in this inpatient role, due to their legal restrictions on controlled drug prescribing. While it was evident that most of the ward staff understood this limitation, there remained the sense that the physiotherapy ACPs lacked the prescribing authority to practice within the full remit and requirements of the inpatient ACP role. This led some to question the practicalities of having physiotherapists in a generalist ACP role, where wide-ranging prescribing is required. Some ward staff were anxious that these prescribing limitations would potentially compromise patient care.
Ward staff highlighted that physiotherapy ACPs were expected to fulfil the same generalist role as the doctors and nurses in the team, but without the prescribing remit of their colleagues. This is an example of the problems that can be encountered when advanced clinical practice is used as a role, rather than considered as a level of practice. As prescribers, both physiotherapy and nurse ACPs in the inpatient medical team are working at the same advanced level, despite their differing prescription remits. However, when thought of as a role, physiotherapists are unable to do all the duties of their nurse ACP peers. To complete an equivalent role to the nurse ACPs, physiotherapist ACPs require the playing field to be levelled to ensure there are no barriers to one professional group over another.
However, despite these findings, physiotherapists undertaking varied advanced roles where prescribing is an essential requirement is not uncommon. Snaith et al (2023) highlight that many ACP roles, which require prescribing as a core skill, are now commonly open to physiotherapists in the UK.
This suggests that the current prescribing legislation for physiotherapists may be ‘out of touch’ with the clinical roles being undertaken by this professional group on the frontline. The varied advanced roles physiotherapists are undertaking need to be recognised nationally to allow the profession to work to its full potential.
One potential solution to the variability of non-medical prescribing legislation across different professions working as ACPs could be the recognition and regulation of the role as a new healthcare profession, where all registered ACPs could have equal prescribing rights and be governed against the same standards.
Staff uncertainty
Ward staff also reported confusion regarding the role of the physiotherapy ACP in the inpatient medical team, and how the role differed from that of doctors and nurse ACPs. Consequently, ward staff stated that this confusion contributed to their preference to work with nurse ACPs and doctors, as they were familiar with their roles. This represents a fundamental problem of current staff perception which, if left unresolved, could fuel the underutilisation and non-acceptance of the physiotherapy ACPs in such teams. Workforce planners should recognise this challenge and work collaboratively with those working as physiotherapy ACPs to establish and agree their role purpose and scope of practice. For example, advanced practice credentials would be a useful aid to help multi-professional ACP teams understand their knowledge/skill bases. Such measures could be cascaded to ward staff to allow all ACPs to be effectively used.
Positive impact
Despite the perceived limitations of physiotherapy ACPs, ward staff viewed them as a clear asset to the inpatient medical team. Their professional background, together with their advanced skills, both improved patient care in the inpatient setting, and enhanced the skill mix and knowledge base in the inpatient medical team and wider MDT.
Ward staff identified that, when given the opportunity to do so, the physiotherapy ACPs provided patients with access to, and aided in the completion of, comprehensive and holistic pain, musculoskeletal and respiratory assessments. This resulted in patients' timely access to expert and specialist care that had not been previously available.
Ward staff also highlighted that physiotherapy ACPs were crucial in advocating for the importance of therapy and rehabilitation on the wards, as well as ensuring that their value was recognised by doctors and nurse ACPs within the inpatient medical team. The ward therapists particularly valued having a therapy advocate in the inpatient medical team. Their addition was seen to bridge a gap, which resulted in enhanced team working between the inpatient medical team and ward therapists, through the forging of strong intra-disciplinary working relationships.
Implication of findings
This study has contributed new knowledge on the benefits and challenges associated with having physiotherapy ACPs as part of an inpatient medical team. The findings can offer insight to teams operating throughout the entire NHS service in the UK, as well as to international healthcare services looking to integrate non-nursing professions into advanced practice roles. These findings can also support workforce planners who are seeking evidence for successful alternative models of care.
Limitations
This form of qualitative research commonly uses face-to-face interviews to gather a rich pool of data (Parahoo, 2014). As such, one limitation of this study was its use of an interview-based questionnaire. While the data collection method used in this study allowed for many health disciplines across the MDT to be included, which provides a more varied pool of data for use in analysis and theme generation, face-to-face interviews could have been included to ensure the greatest amount of data possible were obtained.
Conclusion
This is the first known study to provide an insight into how ward staff in community hospitals experience physiotherapy ACPs working in an inpatient medical team. Physiotherapist ACPs were found to be tasked with generalist duties, used as substitutes for doctors and at risk of loss of professional skills, knowledge and motivation. However, they were also identified to be a positive addition to the inpatient medical team, and reported to play a central role in the advocation of rehabilitation when considering medical treatment decisions and discharges. This demonstrates that physiotherapist ACPs provide value to the inpatient team.
Ward staff also acknowledge that, by being given the opportunity to further use their physiotherapy background within the inpatient ACP role, physiotherapist ACPs could bring greater innovation to the inpatient team. Given the legal restrictions on prescribing imposed on physiotherapists, it is infeasible that they are expected to fulfil the same role as their nursing and medical colleagues, who face no such restrictions. This is a challenge that impacts the role and causes confusion among staff regarding the clinical remit of the physiotherapists. A defined inpatient ACP role that fully uses the physiotherapy ACPs, professional background, skills and knowledge would offer an opportunity for further innovation in community hospitals, while ensuring staff fully understand the remit and scope of the role.


