Exploring the evidence related to the benefits of introducing advanced clinical practitioners (ACPs) to palliative care environments can significantly contribute to the goals of the NHS People Plan 2022/23 (NHS England, 2020) and the NHS Long Term Workforce Plan (NHS England, 2023), and inform on the implementation of new models of palliative care.
In 2016, Imison et al (2016) presented a case for an urgent need to reshape the NHS workforce to meet population demand and the opportunity to train advanced practitioners. Through consolidating existing frameworks from across the UK, and recognising that many advanced practice roles have been developed over the years, it was agreed that a new definition of advanced clinical practice was required. This definition viewed advanced practice as a level of practice, not a specific role, and one that is underpinned by education at master's level (MSc) (Health Education England (HEE), 2017). To establish the need for this research, the question to be answered was: ‘Is introducing ACPs beneficial to palliative care?’
A background literature search was conducted to ensure the research would be current and relevant, using established health databases, including: the Allied and Complementary Medicine Database (AMED), the British Nursing Index (BNI), the Cumulative Index to Nursing and Allied Health Literature (CINAHL), Embase, Emcare, the Healthcare Management Information Consortium (HMIC) database, MEDLINE, PsycINFO, PubMed and the Cochrane Library, using the search terms ‘advanced practice’ AND ‘systematic review’. Overwhelmingly, the research demonstrated a need for organisations and policymakers to standardise competencies, role definitions and scope of practice, which will benefit not only patients but the nursing profession as a whole (Kerr and Macaskill, 2020; Thompson et al, 2020; Hill et al, 2021; Egerod et al, 2021). To unlock the future potential of advanced clinical practice, a clear vision is needed to ensure that ACPs are not left as replacement doctors, but recognised as nurses working towards their maximum potential (Barnwell, 2015). The literature shows that research into the role of the ACP and its benefit to patients, staff and organisations has been conducted in several healthcare settings. However, the analysis of the literature has focused primarily on emergency and primary care. A knowledge gap on the benefits of introducing the ACP to palliative care was, therefore, established.
Aims
The aim of this study was to collect data on the effectiveness of ACPs working in palliative care, identify themes in the literature through narrative synthesis, and provide recommendations for future models of palliative care and research.
Methods
This research was part of an MSc in advanced clinical practice (palliative care); therefore, restrictions relating to how the research could be conducted were necessary to consider. This resulted in the scale of the research being reduced, so as not to undermine its quality. As a postgraduate study, the research followed the methodological stages of a systematic review, with the exception of being carried out by one person and including a limited number of research studies. Due to these exceptions, the research conducted was a systemised review, as defined by Grant and Booth (2009).
The Population, Exposure and Outcome (PEO) search strategy tool (Grewal, 2016) was chosen due to the broad research question. Three search strategies were implemented, with the first focused on the population: palliative care patients. To ensure the spectrum of palliative care was investigated, the terms ‘end-of-life care’ and ‘terminal care’ were included alongside ‘palliative care’. The second, addressing exposure, focused on advanced clinical practice within a job role. As shown in background research, the extensive variety of definitions, job titles and scope of practice within the field of advanced clinical practice had to be considered. ‘Advanced clinical practitioner’ and ‘advanced nurse practitioner’ were chosen as job descriptors, following the Department of Health's (2010) position statement on advanced clinical practice. ‘Clinical nurse specialist’ (CNS) was discounted, due to the established nature of this role and the fact that the terms ‘advanced’ and ‘nurse’ would be included in the search strategies. Finally, to include the outcome measure of benefit to patient care, the term ‘nurse-led care’ was introduced. This would assist in ensuring that nurses or a nursing approach to care was an area within the research. The full search strategy and number of results can be seen in Table 1.
| Search strategy | Boolean operators | Number of results | |
|---|---|---|---|
| Population | Palliative care | (palliative care) AND (‘advanced clinical practitioner’ OR ‘advanced nurse practitioner’) | 41 |
| Exposure | advanced clinical practitioner | ||
| Population | Palliative care | (‘palliative care’ OR ‘end of life care’ OR ‘terminal care’) AND (‘advanced clinical practitioner’ OR ‘advanced nurse practitioner’) | 43 |
| Exposure | advanced clinical practitioner | ||
| Population | Palliative care | (‘palliative care’ OR ‘end of life care’ OR ‘terminal care’) AND (‘advanced clinical practitioner’ OR ‘advanced nurse practitioner’ OR ‘nurse led’ OR ‘nurse-led’) | 789 |
| Exposure | advanced clinical practitioner | ||
| Outcome | Patient care | ||
To create a valid and verifiable narrative synthesis, inclusion and exclusion criteria were established (Table 2). The inclusion criteria of English-language articles were based on the researcher's first language, and research published after 2010 was selected, due to the Department of Health's (2010) most recent position statement regarding ACP roles in the UK. Search results were filtered using three stages: by title, followed by abstract, and, finally, the full text. This process is shown in the PRISMA flow diagram in Figure 1.
| Inclusion criteria | Exclusion criteria |
|---|---|
| In English | Not in English |
| 2010 to present | Before 2010 |
| Country of origin; UK, Europe, North America, Australia. Healthcare systems and advanced practice roles must be comparable to the UK | Outside of the UK, Europe, North America, Australia |
| Must cover palliative care | Palliative care not covered |
| Primary research | Not primary research |
| Peer reviewed | Not peer reviewed |
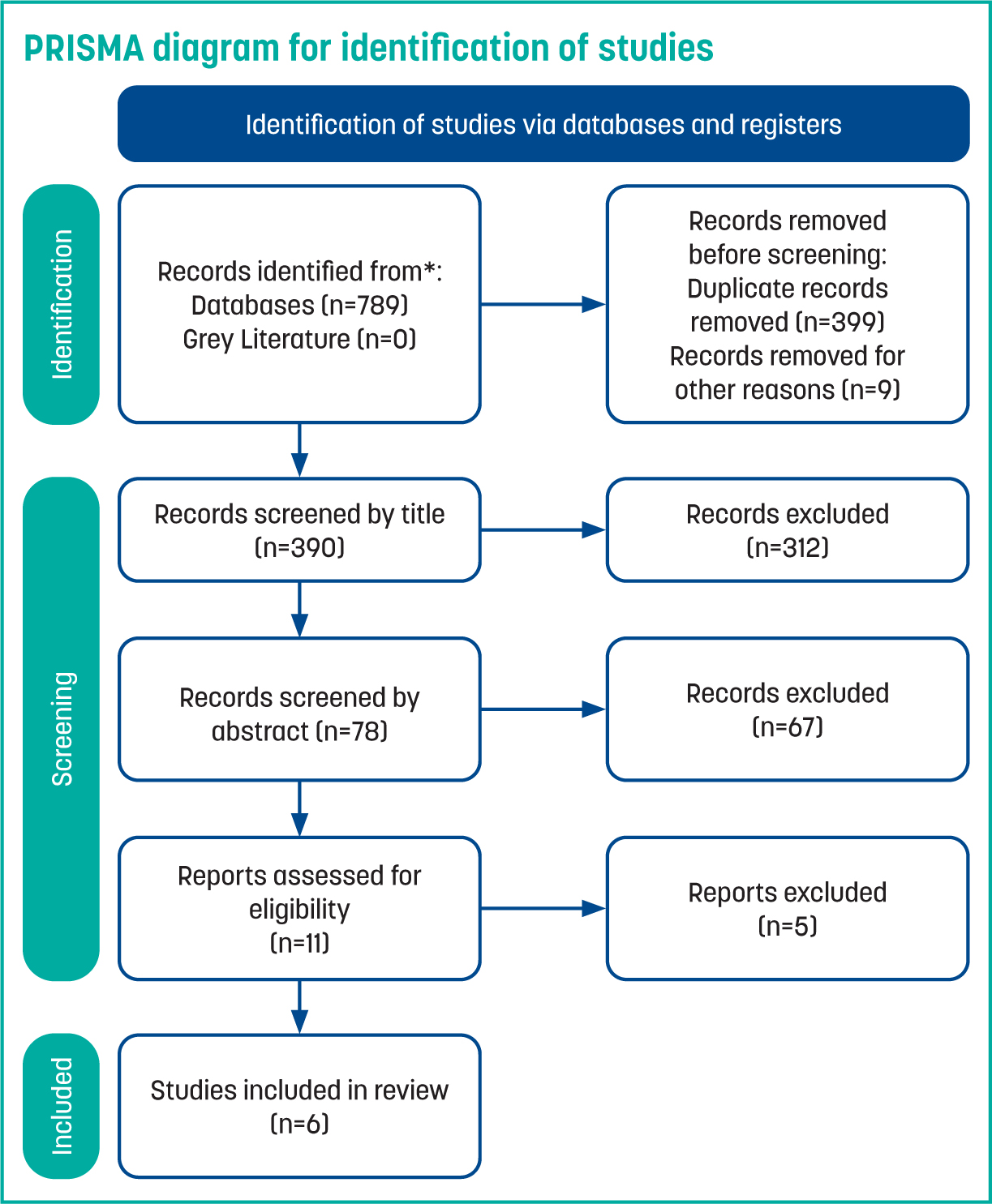
Larrabee's (2009) evidence tables for qualitative and quantitative research were used to review studies for eligibility (n=11). The Critical Appraisal Skills Programme (CASP) (2022) Qualitative Studies Checklist tool was used for selecting and evaluating the most appropriate literature for the review following the initial data extraction from the evidence tables. In order to present evidence-based recommendations for future practice and service improvements, a narrative synthesis approach was used to summarise the data into common themes.
The selection process, which used the CASP Qualitative Studies Tool (2022) to establish quality and relevance of the research, resulted in six eligible studies: four quantitative/mixed method studies and two qualitative studies (Table 3).
| Author | Country | Title | Type of study |
|---|---|---|---|
| Schenker et al (2021) | US | Effect of an oncology nurse–led primary palliative care intervention on patients with advanced cancer: the CONNECT cluster randomised clinical trial | Quantitative, randomised control trial (RTC) |
| Dyar et al (2012) | US | A nurse practitioner directed intervention improves the quality of life of patients with metastatic cancer: results of a randomised pilot study | Quantitative, RTC |
| Kennedy et al (2015) | UK | Fluid role boundaries: exploring the contribution of the advanced nurse practitioner to multi-professional palliative care | Qualitative |
| Imhof et al (2016) | Switzerland | Nurse-led palliative care services facilitate an interdisciplinary network of care | Qualitative |
| Kimbell et al (2018) | UK | Palliative care for people with advanced liver disease: a feasibility trial of a supportive care liver nurse specialist | Mixed method evaluation, feasibility trial |
| Hussain et al (2013) | UK | End-of-life care in neuro-degenerative conditions: outcomes of a specialist palliative neurology service | Retrospective study of clinical records |
Results
Schenker at al's (2021) study aimed to assess the effect of a primary palliative care intervention delivered by oncology nurses on patient outcomes. The experience and practice level of the oncology nurses were not stated, only stating that the participants were ‘designated oncology nurses’. It was assumed that they were working at a specialist level and, therefore, at an advanced nursing level, which justified their inclusion in this research. The randomised control trial (RCT) took place between 2016–2020 with metastatic cancer patients undergoing oncological treatment, with a life expectancy of up to 12 months. A large research cohort (n=672) and multiple sites (n=17) suggests that its results may be generalisable. However, as the research cohort was restricted to one region in the US, the study has selection bias within its population, specifically regarding ethnicity. Results found that there was no mean score difference in quality of life (QoL), symptom burden or mood symptoms of patients in the intervention and control groups. Intensity-adjusted analyses revealed larger estimated effects for patients who received the full intervention, showing that the trial was not successful in delivering what was planned. Many patients did not receive the full intervention due to adherence challenges, workload of nurses and the poor timing of the intervention, which proved to be problematic for the research. The extensive limitations of this research undermines the reliability of the results, when comparing outcomes with other research found in this review.
Another RCT based in the US sought to evaluate the intervention of an advanced registered nurse practitioner (ARNP) on quality of life outcomes of cancer patients receiving discussion-based palliative care (Dyar et al, 2012). The study planned to include 100 participants between November 2008 to July 2009, with the control group not receiving any palliative care intervention. The study was brought to an early close, due to the positive results of the intervention group, as it was deemed unethical to withhold the intervention to palliative patients. Although this action may have reduced the impact of the study, the emotional and mental wellbeing of the ARNP intervention group was shown to have been significantly improved. Dyar et al (2012) have presented a very limited research paper with a unique outcome, featuring an unsuccessful research trial that successfully benefited the participants.
Kimbell et al (2018) conducted a feasibility trial, in the UK, of an intervention to improve care coordination, advanced care planning and QoL for people with advanced liver disease. A weakness in the study design and delivery was that the intervention was not delivered by a specialist or ACP palliative nurse. The study specified the roles and responsibilities of the liver specialist nurses that encompassed the pillars of advanced clinical practice. While this role may be comparable to the role of the ACP, it does not relate to the field of palliative care. The study showed that a nurse-led intervention improved people's QoL, facilitated care coordination with multiple healthcare professionals, reduced hospital admissions with advance care planning and improved updating of summary care plans. However, while a thorough methodology through use of a mixed-method design, standardised tools and impartial interviewing strengthened the rigor of the research, the study failed to explore the benefits of the ACP role in palliative care due to the inexperience of the nurses within the field.
Hussain et al (2013) presented a UK-based research assessing outcomes of a nurse-led palliative neurology service against the National End-of-life Care Programme (NEoLCP) 2010 framework. A CNS in palliative neurology coordinated multidisciplinary care for patients (n=62) between December 2006 and April 2012. The written evidence provided by the CNS shows that they were working at a level of advanced clinical practice that was incorporating the four pillars of advanced practice (HEE, 2017). Hussain et al (2013) showed that a nurse-led service of specialist palliative care reduced hospital admissions, increased hospice admissions for a place of death, reduced the impact on NHS services and achieved the goals set out by the NEoLCP framework. Hussain et al (2013) produced a reliable and rigorous study that demonstrated that a CNS, working at an advanced clinical practice level, can help services meet national guidelines.
Imhof et al (2016) presented a Switzerland-based qualitative study, which adopted a grounded theory approach and used semi-structured interviews (n=41) to gather data from carers, healthcare professionals, organisations and politicians. Through thematic presentations of findings entitled ‘spheres of action’, a clear representation of the ACPs positive impact was shown through their ability to clinically assess and gauge complex palliative situations including medical conditions, care needs, living and social needs. The study was limited by the inclusion of non-specialist palliative care nurses, which clouded the immediate applicability of the results to the pursuit of this article's research question. The strength of Imhof et al's (2016) research lies within the exploration of the impact that the specialist nurse has on all areas of palliative care, including their impact on the service as a whole, other healthcare professionals and host institutions.
Kennedy et al (2015) specifically evaluated the role of advanced nurse practitioners (ANPs) within palliative care. Competencies and core areas of work were explored over a 10-month period. Participants included members of a specialist palliative care unit (n=21), ANPs (n=2), multi-professional staff (n=14) and patients/carers (n=5). Though the total number was small, the study captured a broad range of opinions and evidence. The ANPs discussed how their experience and education level, specifically their MSc in Advanced Practice, prepared them to work in clinical assessment, prescribing, education, leadership and research. Data were collected between June 2010 and March 2011. A qualitative study design was used to facilitate an iterative process that took the ‘participatory, evidence-based, patient-focused process for guiding the development, implementation, and evaluation of advanced practice nursing’ (PEPPA) framework for implementing and evaluating ANP roles into consideration (Bryant-Lukosius and Dicenso, 2004). The main theme extrapolated from the data was their unique contribution to service delivery, as they crossed the traditional boundaries of nursing and medicine through the ability to ‘care and treat’ patients. This showed their potential to enhance specialist palliative care through the fluid role boundaries of the ACP. The relevance to clinical practice from a stakeholder perspective was explored, establishing that success and sustainability of the ACP role relies on organisational support of the role. A small snapshot reduces generalisable results but produces a strong foundation for future research, especially since the HEE (2017) framework was established after this study was published.
Discussion
This research analysed 11 research papers that met the inclusion criteria; six were selected for review. The six selected studies used several different research methods: two RCTs, two qualitative studies, one mixed-method feasibility trial and one retrospective study of clinical records. A narrative synthesis enabled for the comparison of research with differing methodologies and outcome measures within varying areas of palliative care and varying countries of origin including the UK (n=3), US (n=2) and Switzerland (n=1). Benefits ranged from the patient perspective to healthcare professionals and stakeholders; however, only one of the studies included the combination of an established palliative care service with an experienced specialist nurse working at an advanced level (Imhof et al, 2016). All other studies either researched a new intervention with an experienced practitioner in their field or inexperienced ACPs. All the selected studies had strengths and weaknesses in their comparability, with the final selection reviewed and results analysed through a narrative synthesis perspective. Three themes were extracted from the systemised review.
Theme 1: nurse-led management of care
The most dominant theme throughout the systemised review was the nurse-led management of care, with all research being led by ACPs, albeit in different role titles and specialities. It could be argued that all nurses fulfilling the lead role within the research could be seen to be working at an advanced clinical practitioner level.
A nurse-led model of care and continuity of care were the main described possibilities and impacts of the ACP role. Both Kennedy et al (2015) and Imhof et al (2016) found that a nurse-led model of care was beneficial, not only for patient care, but for staff and organisational structures. The high standard of patient management enabled evidence of reduced GP contacts, hospital admissions and hospital deaths (Hussain et al, 2013; Kimbell et al, 2018). The high level of skill demonstrated and delivered across the education, leadership and management pillars, as well as the benefits added to care and on patient QoL, was shown to be attributed to the ACP's capacity to coordinate the multi-dicsiplinary team.
Theme 2: benefit to patient care
Quality of life
Dyar et al's (2012) study produced results of such high significance that the researchers decided to stop their trial, as it was deemed unethical to withhold the palliative intervention when it was clearly having a benefit to the QoL of patients. This is supported by Kimbell et al (2018) which showed that the specialist nurse working at an advanced clinical practice level generated significant improvements in patients' QoL.
Advance care planning
The ACP's clinical management and advanced communication skills were shown to assist in specific areas of palliative care. Hussain et al (2013) states that 95% of patients in their study were reviewed for capacity and advanced care planning, with 40% (14/36) going on to have cognitive impairment and being unable to express their wishes at the end of life.
Theme 3: more time
ACPs were able to dedicate more time to patients and colleagues, which resulted in cost-effective services that did not replace, but rather complimented, members of a team; this factor helped improve service delivery and outcomes. The ACP was shown to build trust with patients, help remove the ‘time pressures typical of medical appointments’ and allow patients to feel that they were getting more of a ‘chance to speak’ and ‘getting more answers’—all features that are vital and important in the provision of end-of-life care.
Cost-effective
This research has found that the ACP in palliative care has a financial impact through optimising the use of resources and reducing hospital admissions, GP visits and outpatient non-attendance (Hussain et al, 2013; Imhof et al, 2016; Kimbell et al, 2018). However, Kennedy et al (2015) suggested that the ACP can not function as a replacement for existing GP services and that they are able to deliver ‘a unique contribution’ and ‘complement existing medical models’.
Education
Education was delivered by those leading the research interventions to patients, carers and colleagues across a number of studies.
Conclusion
This article demonstrates that the practice of nurses working at an advanced clinical level is in its infancy within palliative care. Further research is needed on the impact of nurses educated to an MSc level in advanced clinical practice compared to established CNSs. Recommendations for clinical practice extrapolated from the reviewed studies in this article mirror those found in previous research, which emphasise that the ACP role within the workplace needs to be further defined, and nurses need to be encouraged further to continue to work at an MSc advanced clinical practice level. Further research into professional regulation of the ACP could support the literature regarding the definition and scope of the role. This research has shown that the role of the ACP is beneficial to palliative patient care, staff and organisations.


