The field of advanced practice is a developing area within the NHS. Advanced practice has been defined ‘as being delivered by experienced, registered health practitioners’ (Health Education England, 2017). The level of practice is characterised by a high degree of autonomy, which is underpinned by the four pillars of clinical practice: leadership and management, education, research and clinical competence at an advanced level in a specific area. Current evidence in this area (Lefmann and Sheppard 2014; Morris et al, 2015) focuses on the impact of musculoskeletal interventions, which have benefits for patients with soft tissue injuries, minor fractures and balance issues (Crane and Delany, 2013). Therefore, this article aims to explore the impacts of a trainee advanced practice physiotherapist (tAPP) assessing patients with frailty in the emergency department (ED).
Advanced practice for physiotherapists is an evolving area, in part because of increasing pressures on EDs in developed countries. Extended scope of practice physiotherapy roles have been established in the UK since the mid-1990s. One of the key reasons for the creation of these roles was to accommodate the changes introduced by restricted working hours for doctors (McClellan et al, 2012). An increase in patient attendances over the last decade (Lowthian et al, 2012) has driven changes and innovation in the utilisation of hospital resources and services within the existing workforce (Lowthian et al, 2011). Patients with frailty often present to the emergency department in a non-specific fashion or with frailty syndromes such as falls, delirium, immobility, incontinence, carer strain and social breakdown of care (Ellis et al, 2017). Older patients present to the ED because of the increased likelihood of multiple comorbidities, such as ischaemic heart disease, diabetes, hypertension and Parkinson's (Barnett et al, 2012) and are at a greater risk of acute illnesses.
Physiotherapists were secondary contact practitioners in Eds until recently, completing assessment, treatment and discharge planning after an examination by an ED doctor (de Gruchy et al, 2015). Concerns have been documented around physiotherapists being a first contact for patients; these include the risk of overlooking serious medical conditions and the possibility of an adverse event if initial screening by a doctor is omitted (Fleming-McDonnell et al, 2010). However, it has been shown that physiotherapists can independently distinguish medical conditions originating from musculoskeletal issues and can manage these pain issues in first-contact situations (Stowell et al, 2005).
Physiotherapists can apply specialised knowledge in clinical reasoning and treatment in both emergency presentations and longer-term chronic conditions within clinical settings (Sullivan et al, 2011). A large study conducted in 2012 with 5,000 participants, hypothesised that early frailty assessment and therapy could increase the likelihood of early discharge. It was found that benefits were more closely linked to musculoskeletal presentations, primarily because other presenting complaints required hospital admission (Arendts et al, 2012). The study also found ‘early use of multidisciplinary allied health input influences hospital admissions rates in a small number of diagnoses’ (Arendts et al, 2012).
While existing evidence highlights the benefits of therapists serving as first-contact practitioners in advanced practice roles, and of physiotherapists conducting frailty assessments in the ED, there is limited data on the combined role of a physiotherapist in an advanced practice position who assesses both the medical and social aspects of frailty in patients. This study aims to evaluate the effectiveness of advanced practice physiotherapists in assessing and treating patients with frailty within the ED. Specifically, it will focus on reviewing wait times to be seen by a practitioner, reducing the length of time patients spend in the department, and decreasing the time required to develop an appropriate treatment plan, including medical and discharge planning.
Aims and objectives
The aim of this study investigates the impact of a tAPP review of patients with frailty in the acute setting, as part of the physiotherapist role extension.
Methodology
Study Design
This study was designed as a normative experimental comparative study (Bukhari, 2011) involving quantitative data collection (Mills et al, 2006). All patients in the control group were seen by an ED doctor and received a separate therapy assessment from an occupational therapist or physiotherapist in September and October 2020.
The intervention group received an assessment carried out by a trainee advanced physiotherapy practitioner (tAPP) encompassing both medical and therapy components to establish medical status and a potential discharge plan in September and October 2021.
Advanced physiotherapy practitioner role
At the time of the study, the advanced physiotherapy practitioner was still in training, with competence demonstrated in clinical assessment and diagnosis, however modules surrounding prescribing and radiology request had not yet been completed. The tAPP has an extensive background working with older patients with frailty, incorporating therapy assessments and complex discharge planning within the ED.
The tAPP was supervised by a senior colleague, either an ED consultant or a specialist registrar during the study period. This supervision consisted of case-based discussions or senior reviews in the case of more complex patients.
Study population
The study included patients attending ED, aged over 65 years, with the need for therapy or an element of frailty identified on assessment. All participants provided consent for the intervention. The tAPP prioritised seeing these patients, where possible, while balancing the remaining ED caseload. Baseline data were assembled using previous data gathered during therapy assessments carried out between September 2020 and October 2020. These cases were previously identified to have a degree of frailty as well as therapy needs. All these patients were seen by an ED doctor before therapy intervention.
Data Collection
Retrospective data were obtained to formulate the control group, while data collected throughout the study period were used to establish the intervention group. All participants had their details logged when they attended the ED, including the time of arrival and departure from the ED and time when seen by a practitioner. No further information was needed to allow a comparison to the control group. Data for the intervention group were collected over a period of 5 months, from April to August 2021.
Ethical considerations
Before data collection began, ethical considerations were addressed through the University of the West of England's ethics process, and all risks were mitigated. All GDPR regulations were strictly followed. Full disclosure was provided to each participant, and verbal consent was obtained from the emergency medical practitioner for the intervention group, and from both the emergency medical practitioner and physiotherapist for the control group, prior to the assessment
Data analysis
Data were analysed using the numbers programme by Apple Inc. Raw data were input into the system and comparisons were made using averages.
Results
The tAPP completed approximately 114 hours of clinical practice between 16 March 2021 and 31 August 2021. A total of 65 patients were seen and 39 patients were excluded from the data analysis because they did not meet the inclusion criteria (Table 1); 25 patients were included in the data analysis. All patients' notes were reviewed using Medway and Electronic Documents and Records Management to find the timings of plans being established.
| Inclusion criteria | Why? | Exclusion Criteria | Why? |
|---|---|---|---|
| Aged over 65 years | Specialist area for advanced practice physiotherapists | Aged under 65 years | Not an area of expertise for advanced practice physiotherapists |
| Therapy needs identified on assessment | To allow direct comparison to control group | Acutely unwell patients | Not within the current scope of the trainee advanced practice physiotherapist |
| Element of frailty identified on assessment | To allow direct comparison to control group |
Control group: assessment by an ED practitioner (Foundation Year 2 or above) followed by a therapist assessment (occupational therapist or physiotherapist).
Intervention group: medical and social assessment completed by a tAPP (Table 2). Review waiting times were included to provide an indication of the pressures on the department at the time of patent attendance monitoring. In the control group, patient waiting time to be seen by an ED practitioner averaged at 76 minutes, in comparison to 137 minutes for the intervention group (Table 3). These times are greater in the intervention group possibly because of the impact of COVID-19 on ED attendances.
| Female | Male | |
|---|---|---|
| Intervention group | 18 | 7 |
| Control group | 14 | 11 |
| Intervention group | Control group | |
|---|---|---|
| Wait to be seen (minutes) | 137 | 76 |
| Time spent in the emergency department (minutes) | 503 | 433 |
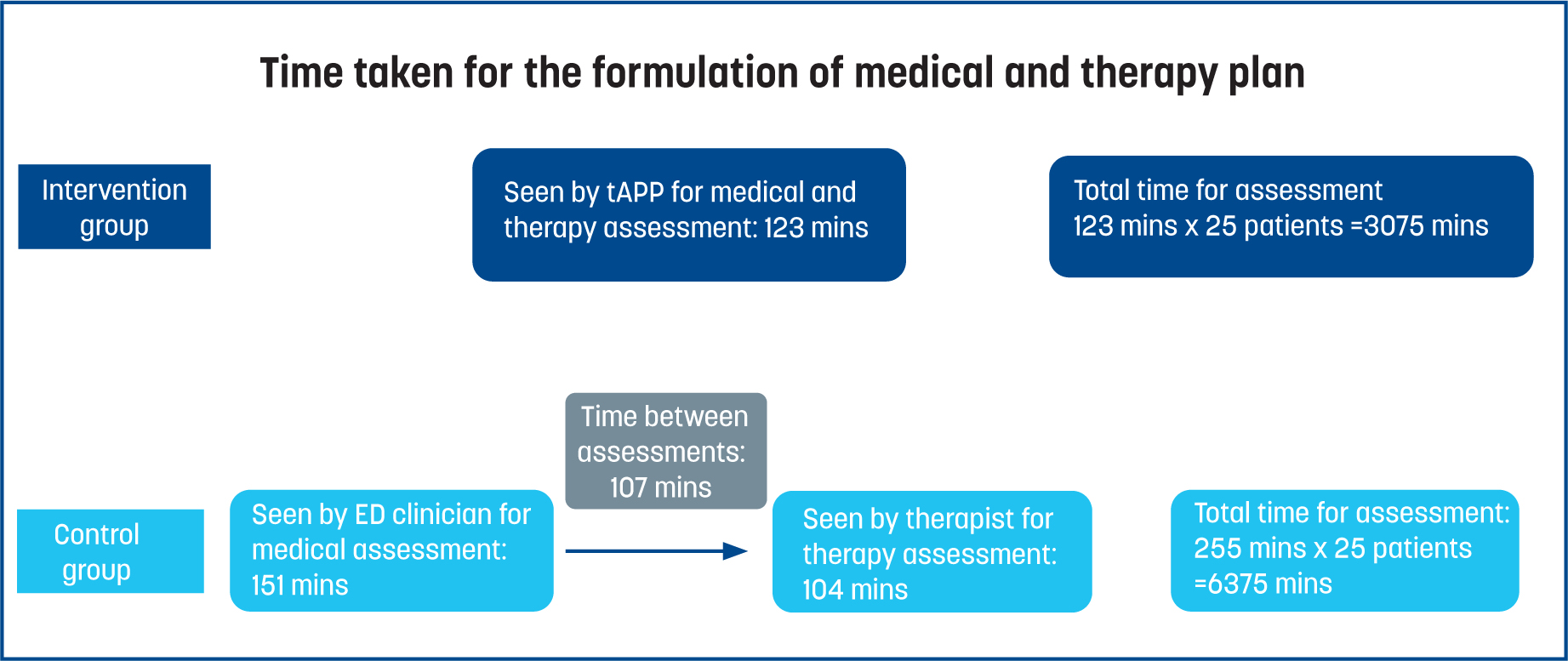
Patients in the control group, seen by an ED doctor (at Foundation Year 2 level or above), received a medical plan 151 minutes after the assessment began. In contrast, patients seen by the tAPP received a medical plan 123 minutes after the assessment began. A total time saving of 91 minutes, equating to 2,275 minutes (37.9 hours), was achieved across the 25 patients seen. In the ED, patients are typically seen in order of arrival, with only acutely unwell patients being prioritised. Patients seen by the tAPP also had a therapy plan formulated 123 minutes after the medical assessment had been completed, compared to 275 minutes for the control group. In the control group, 20 patients were seen by a therapist post medical review, where the average length of time between a patient's medical and therapy assessment was 107 minutes. This suggested that assessments were conducted consecutively rather than concurrently, as in the intervention group (Table 4 and 5). The calculations show that both assessments were completed in an average of 3075 minutes for the intervention group, compared to 6375 minutes for the control group (Figure 1). This equated to a total difference of 3300 minutes for all 25 patients; 55 hours of time saved throughout the study period. The mean waiting time of 107 minutes between the ED medical and therapy assessment amounted to an additional 2675 minutes of patient waiting time (44.5 hours).
| Intervention group | Control group | |
|---|---|---|
| Time since arrival (mins) | 259 | 228 |
| Time since consultation (mins) | 122 (13-270) | 151 (23-363) |
| Intervention group | Control group | |
|---|---|---|
| Time since arrival (mins) | 260 | 351 |
| Time since the start of assessment (mins) | 123 | 104 |
| Time since medical consultation (mins) | 123 | 275 |
Discussion
This is one of the first studies to explore the impact of a tAPP reviewing patients with frailty within the ED. Existing research is more focused on musculoskeletal skills of physiotherapists working within advanced practice, as opposed to the other interventions assessed in this study. Exploring primary data on the ‘wait to be seen’ and ‘length of stay’ for patients in this study allowed for an assessment of department performance during the timeframe of the patients' ED visits. The results showed that, in 2021, patients in the intervention group waited on average 61 minutes longer to be assessed and spent an additional 70 minutes in the department compared to the control group from 2020.
This is likely indicative of the impact of the initial wave of COVID-19. A comparative study found a 50.7% decrease in first-time ED attendances at King's College Hospital in 2020, compared to 2019. This was determined by reviewing records of all first-time attendances during the lockdown period and comparing them with those of the previous year (Kociejowski et al, 2021). One view is that acutely unwell patients avoided emergency services during this time. It has also been suggested that better bed planning, increased telehealth and community appointments, alongside the reduction in demand, resulted in decreased length of stays within ED during 2020 (Woodruff and Frakt, 2020). This was possibly a contributing factor in the reduced times for assessment, evidenced in the control group. However, the patient attendance group with people aged over 65 years was not impacted during the COVID-19 pandemic (Vollmer et al, 2021), which was the tAPPs' targeted review group in this study. It is essential to take this into consideration when aiming to reduce workload demands on existing service.
All assessments carried out by the tAPP were discussed with a senior clinician, who assessed the patients before discharge. Requests for imaging and prescriptions of any medications were completed by the senior practitioner (ED consultant) because the tAPP had not yet completed the relevant clinical modules and associated competencies. This meant that adequate support was provided to the tAPP throughout the study period. As these modules are completed, the time taken for the tAPP to assess patients may reduce further, as they would be able to work more autonomously in prescribing medications and requesting relevant imaging. This means that a qualified APP could help to reduce assessment times. The service would benefit further by enabling tAPPs to specialise in assessing patients with frailty.
According to literature, clinical and situational learning is considered vital to professional development of students (Chartered Society of Physiotherapy, 2002). This concept resonates with trainees in advanced practice, where a minimum threshold of clinical hours should be determined to expand clinical competence and confidence. While the scope of the tAPP was maintained throughout the data collection period, it is worth noting that advanced practice is designed to transform and modernise pathways to enable the safe and effective skills across what are seen as traditional professional boundaries (Health Education England, 2017).
The benefits of therapists working in emergency departments has been evidenced previously. For example, James et al (2016) found that these assessment reduced unnecessary hospital admissions particularly for older patients. Advanced clinical practice roles in healthcare can enhance patient-centred care for the patients, and as a result, assist in increasing patient flow efficiency (NHS, 2019). Review data highlighted that patients requiring both therapy and medical assessments had their plans formulated in 123 minutes, as opposed to 255 minutes when performed separately by the ED clinician and then a therapist.
When continuous care is provided, it enhances patient satisfaction and enables the doctor to gain valuable insights, which helps save time in information gathering, reduces the need for unnecessary laboratory tests and improves the management of patient expectations (Hjortdahl and Borchgrevink, 1991). Enabling the tAPP to complete both aspects of the assessment resulted in a reduction in the duplication of tasks, such as consultations involving patient, relatives or carers. Consequently, in-patient admission assessment or discharge requiring community follow up was established earlier in the assessment process. This is evidenced in the mean plan formulation time of 91 minutes per patient. The precise benefit of reducing patient attendance time is difficult to quantify. However, published literature has demonstrated that a less crowded ED has a broad range of positive impacts, including decreased mortality, reduced readmissions, improved patient satisfaction, lower staff stress levels and shorter patient stays, both within the ED and throughout the hospital (Morley et al, 2018).
Overall, tAPP frailty assessment intervention resulted in a time reduction, where therapy and medical assessments were completed in 123 minutes, compared to 255 minutes per patient in the control group. A total time-saving achievement of 3300 minutes within the study period is an important initial step in exploring avenues to further enhance ED efficiency and establish other dynamic ways to expand the physiotherapy role further.
Strengths and limitations
Since this was a novel undertaking and exploration, research around this area was limited. As a result of clinical delays, retrospective data were used to complete the study within the researcher's planned timeframe. The sample size of this study was small, a clear limitation to this study. Steps were taken to make the data as comparable as possible, and to minimise the impact of external factors. Since the study was carried out by the tAPP, there is a possibility of potential researcher bias. The use of numerical outcome measures minimised the effects of research bias by eliminating subjective opinions regarding the data.
Conclusions
The study investigated the efficiency of a physiotherapist role extension intervention within the ED setting. Physiotherapists working in advanced practice roles is still an emerging field that requires further research. Although this study had a small sample size, patterns can still be identified from the data. Since the tAPP was still in training, ED clinicians clearly supported the assessments to ensure patient safety. Data collection indicated a time saving of 57.5 hours during the study period, across the assessment of 25 patients with frailty, with the tAPP completing assessments in the ED. While the exact benefits are difficult to quantify, the time savings and the assessments conducted suggest that there may be improvements in continuity of care, reduction of work duplication and earlier formulation of medical and therapy plans. Further research into patient outcomes could be valuable to continue demonstrating the effectiveness of physiotherapists in advanced practice roles.


