Health Education England (HEE) published its Multi Professional Framework in 2017 (HEE, 2017). The framework aimed to develop a national consistency of advanced clinical practice and was underpinned by the four pillars of advanced clinical practice. The research pillar of the ACP HEE framework highlights that those working at an advanced level should be engaged in research activity.
The goals of evidence-based practice are to establish consistent practice (in accordance to the latest research findings) and create change (Titler, 2008). As ACPs tend to be the static workforce within an area, the ability to appropriately critique evidence and challenge current practice is key to ensuring departmental, individual and professional development.
Therefore, ACPs are an important driving force when implementing change through identifying current knowledge gaps and areas requiring improvement. Through synthesising from relevant research, ACPs can use the current evidence base to underpin their actions and inform practice.
Fothergill et al (2022) completed the first large-scale evaluation of advanced practitioners nationally and recommended that increased efforts are needed to support ACPs with research engagement. The mixed-method online survey of ACPs concluded that the research pillar was a neglected area of focus, with less than 11% of ACPs actively involved in research. The authors defined ‘research’ to their participants as: audit, research, quality improvement, service evaluation and the economic evaluations of practice. Previously, there had been no exploration to identify why this pillar was underrepresented.
Background
Nottingham University Hospitals (NUH) employs over 180 qualified and trainee ACPs. Within NUH, there had been feedback that although trainee ACPs had a clear training structure and programme, upon qualifying, there was no clear guidance or direction for the role. Therefore, the trust has refocused on ensuring that the progression of qualified ACPs remains within all four pillars of advanced practice. Three steering groups were formed to address ACPs opportunities to progress within leadership, education and research and innovation. Steering groups consisted of ACP volunteers who had a particular interest in each area, with their focus being how to engage ACPs in their respective pillar and to plan a progress map for the first 5 years after qualifying.
From the initial steering group meetings, it was noted through discussion and exploration of each clinicians experiences that research and innovation was the area with the least amount of interest. ACPs who did have an interest in this pillar often described feeling isolated and unsure of how to progress or encourage engagement of others. As individuals who had volunteered to be part of a research focused group, the authors understood that they were unlikely to understand why other ACPs did not share their enthusiasm towards research and further evidence gathering from the wider ACP workforce would be required.
Methods
A questionnaire was designed by the Research and Innovation (R&I) ACP team and conducted at the 2021 NUH ACP conference. The questionnaire was written by two members of the R&I steering group, then reviewed and approved by other members in advance of the conference.
Ethical approval
A questionnaire tool designed by the UK Medical Research Council (UKMRC) and NHS Health Research Authority (HRA, 2020) was completed to determine if ethical approval would be required (UKMRC, 2020). The study was confirmed to be in keeping with research, as the results were going to be generalisable and the conclusions were hoped to be transferrable to other settings, such as other ACPs and other NHS trusts. A second questionnaire, signposted and written by UKMRAC and NHS HRA (2020), must be completed for projects which are considered research. This questionnaire was completed and it was concluded that the authors did not require an NHS Research Ethics Committee (REC) review.
Participation
There were no financial or other incentives to participate in this study. Participants were free to decide whether they wished to participate. Informed consent for personal responses for research purposes was assumed, as the survey was optional and highlighted to be completely anonymous.
Personal identifiers were not available to the research team. The questionnaire employed both quantitative and qualitative aspects to reflect the aims of the R&I steering group, in order to gain a multidimensional understanding of the ACP's perception of research. Questions asked included:
- Whether the ACPs felt they were currently engaged with research
- How they felt towards research
- Their opinion of what stopped them accessing and engaging in research.
The questionnaire was included as part of an interactive presentation run by the R&I steering group. The focus of the session was to provide data that could be utilised by the group to gain a better understanding of how the research pillar was viewed by ACPs, in order to develop strategies to address them. During the presentation, ACPs were provided with a code that directed them to an anonymous online questionnaire to complete on their personal devices. In total, there were 73 responses from approximately 110 participants who were present at the time of this session; responses were recorded using the online survey tool.
Review of the responses identified key issues relating to their perceptions of research including:
- Apprehension of critiquing evidence
- Feeling overwhelmed by the vastness of the current evidence base
- Poor understanding of how to demonstrate critical engagement in research.
Similarities between the findings of Fothergill et al (2022) were apparent, with 62% of respondents reporting that they were not actively engaged in research within their current ACP role.
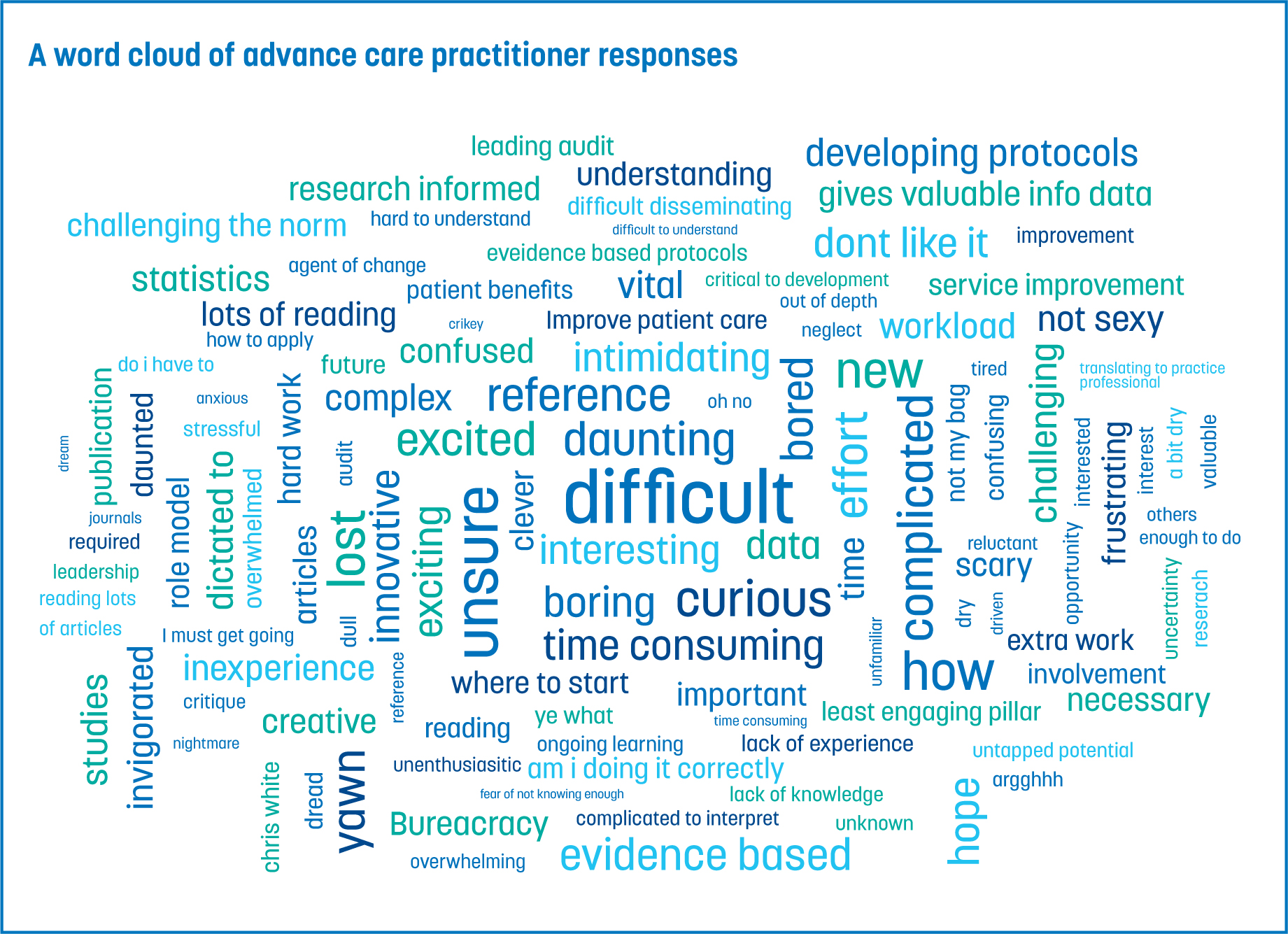
There was no set definition of research provided, but examples were given (but not limited to) such as audit, research delivery and production of local guidelines. There was an overwhelmingly negative response towards research and a sense that journal articles and new evidence were inaccessible. When asked to describe their feelings about research and innovation using 1–3 words (Figure 1), the most common phrases and themes that emerged were ‘daunting’, ‘difficult’ and ‘intimidating’.
Participants were asked how the R&I steering group could support development within the R&I pillar. Several responses centred around building confidence within the research pillar; other participants highlighted the need for online resources to be made available (Table 1).
Table 1. Advanced Care Practitioners Asked How the Research and Innovation (R&I) Steering Group Could Support Their Development Within the R&I Pillar
| Category |
|---|
| ‘Just examples of critiquing articles’ |
| ‘Where to start when approaching a paper…a dummies guide!’ |
| ‘Literature searching skills’ |
| ‘…an online library of how-to guides and critiquing skills’ |
| ‘…a journal club podcast’ |
From this feedback, it was concluded that the main barrier to ACPs engaging with research was poor confidence and finding research difficult to approach and access. Using this information, the R&I group met to decide on a plan to address these issues. There is a wealth of free information available online, including critical appraisal tools, podcasts and blogs that summarise articles. As this was already available, signposting alone was unlikely to make a significant difference in engaging ACPs in research. The steering group did not want to just show adherence to a pillar within a personal portfolio, but wanted to make an active difference in order to open the world of research to the ACP team. Therefore, an active intervention was required; this need resulted in the creation of the NUH ACP journal club.
With the evolution of easily accessible research and its dissemination through email and social media, it can be easy to be swept away by a key conclusion or striking abstract (Bolderstone et al, 2018). This can often be reinforced by those who are in a position of authority promoting such research. To be critical and sceptical is key in these instances.
Reinforcing the need to step back from a piece of evidence and examine how their conclusion was gained is key to ACPs; however, it is also a skill that requires education to develop. Furthermore, it is commonly thought of as difficult. Currently, there is wide variation in the training and experience of ACPs across the UK, although this is currently being addressed by Health Education England's Centre for Advancing Practice. Therefore, the ACPs level of research education and experience of critical analysis will vary between individuals based upon their previous experience and their initial professional training
Traditionally, journal clubs were held face-to-face, with an expectation that everyone had read the paper and had a pre-existing wealth of knowledge of critical appraisal. As stated by Mohr et al (2015), the journal club concept was initially introduced to review pertinent practice-changing articles. Realistically, in 2023, this is not a feasible approach because of the sheer volume of new evidence emerging daily. Therefore, the NUH ACP journal club aimed to improve upon critiquing and appraisal skills to use when addressing the quantity of available evidence.
Results
To increase the confidence of learners, it was felt that the ACP journal club should be ACP-led, with ACP presenters. The temptation was to ask experienced researchers and academics to present, however, it was felt that this would discourage participation and decrease confidence of attendees, because of the advanced knowledge of the speaker potentially creating a perceived hierarchy.
The didactic style of journal clubs is not an effective learning environment (Chetlen et al, 2017). A peer-based learning environment minimises the risk of power differential with staff who are perceived as more senior, which can create a reluctance of less experienced staff to offer an opinion (Bolderstone et al, 2018).
The R&I steering group felt that putting these individuals into an environment with unknown medical speakers and asking them to be vulnerable was unlikely to succeed. Collaborative learning approaches are proven to be more effective than a direct instruction style (Hänze et al, 2007). Therefore, a peer-learning approach was adopted to ensure the ACP learners felt comfortable and confident in a peer-supported group. The ‘flipped classroom’ approach requires that learners come to the sessions having already attempted their own critique. This creates an active learning environment, rather than relying on a passive listening approach, which is proven to improve learning (Hew and Lo, 2018).
Within the NUH ACP cohort, there are varying abilities with regards to research understanding. However, further dividing these groups up to create two different sessions did not seem practical or beneficial. A peer-learning approach of a mixed ability group is key to improving confidence and enhancing the learning experience for others. Wegner (2010) reports that the lesser experienced learner feels a need to align their experience with the competence of their more knowledgeable peer and will subconsciously strive to achieve this.
The opposite effect also occurs when the more experienced member becomes aware of their peers' situation and wants to assist in their learning (Wegner, 2010). The competence of the higher-level student pulls the lesser experienced learner in line with them (Wegner, 2010). Therefore, an ACP-led journal club was created, aimed at all abilities, with the common goal being to engage more ACPs within critical appraisal and research.
Another element to the design process was the subject of the article to critique. With ACPs from over 20 specialities, it was difficult to find articles of common interest. However, this could be considered advantageous, as the focus would be on critical appraisal, rather than the temptation to discuss the intricacies of the clinical impact. In turn, this would allow for the journal club to be opened up to multiple specialities and professions with one common goal, to improve upon their critical appraisal skills and improve access to research.
Successes
Logistically, in a post-pandemic world within NHS Trusts, finding a physical space to host several people is often the most challenging aspect of a group event. Having an online platform to host a journal club has enabled greater attendance through ease of access and reduced time away from clinical duties.
This is particularly pertinent at NUH, where the campuses are spread over two sites which are 2 miles apart. Not only does the online platform aid the group participation geographically, but the various functions available allow for ACPs to access education at their convenience around busy clinical schedules.
Meetings are recorded, with consent obtained from all participants prior to joining the session, and made available on the intranet site along with a link to the paper, which was appraised. The online platform also helps aid a structured approach.
Instead of an expert leader, the use of a facilitator, to maintain order and promote flow, allowed greater opportunity for participation and building confidence within participants (Cranley et al, 2017). For example, the use of the ‘hand up’ function facilitates an organised approach to participants' responses, rather than in a face-to-face setting, where the more confident participants can dominate the conversation unintentionally. Having a dedicated turn-taking format within the relative comfort of familiar surroundings enhances confidence to share an opinion, which further enhances the collaborative learning experience.
Challenges
There were negatives to this approach, such as establishing an adequate internet connection, having a device with a microphone, camera, speaker and a screen that is large enough to see the content. However, as the use of online platforms becomes the new norm, the authors have found that technological disruptions have lessened and common fixes are widely known for the majority of issues. The group has also been able to utilise technology in the form of social media to promote awareness of the journal club and increase participation.
Another issue that was expected, yet not anticipated to be so persistent, was the small number of ACPs willing to present. ACPs enjoyed participating with around 30 ACPs (20% of the total NUH ACP workforce) regularly attending the sessions. Feedback was collated anonymously using an online survey and ACPs reported that they found the sessions very beneficial. They stated that their understanding and confidence in research had improved, yet there was little interest in volunteering to present a session.
The presenters ended up coming from a small pool of individuals who were happy to present on a regular basis. Various techniques were employed to increase the number of people willing to present. These included offering to co-present and co-write presentations, but this did not gain any positive responses.
Certificates for presentation were awarded to those who did present and a journal club ‘handbook’ was created, which highlighted the aims of the journal club, to increase confidence within research and the expectations of participants and presenters.
The handbook included a template of how a journal club session may be created and included a suggested layout and a large glossary of phrases and terms to break down the inaccessible concept of research. The handbook was put on the trust intranet for all to access and received a positive response. However, there has been an ongoing issue in finding more ACPs to present, with little change in the reasoning for this, the ACPs feel they are not confident enough to present. This insight has been gained from sending anonymous feedback forms to ensure adaptions are made to the responses.
Discussion
From a peer-based learning environment and initiative, the common misconceptions of research identified in the initial questionnaire were able to be addressed. From pre-intervention feedback at the NUH ACP conference (2021), it was clear that research was felt to be inaccessible, complex and filled with statistical jargon. However, from the learners immersing themselves in critical appraisal in a group environment, those misinterpretations appear to be resolving based upon the anonymous feedback gained from the initial journal club sessions.
The alteration of their usual learning environment of lunchtime lectures or online webinars has positively addressed ACPs views towards research and of their ability to appraise the current evidence base. Seeing their peers taking on a leading role at each session highlighted that they did not need to be an expert within research to critique a paper. The model of each individual being transparent with how they completed their critical analysis, often by using a critiquing tool, triggered greater engagement as confidence quickly grew.
Alongside the improved confidence within research that was reported in the feedback, the use of a virtual journal club allowed for all participants to hone their skills of presentation and effective communication in a novel way. This was another unintended benefit of a peer-based non-traditional journal club.
Implications for future practice
NUH is one of the largest employers of ACPs, with a varied mix of clinical backgrounds. Therefore, it could safely be reasoned that most themes uncovered at NUH are likely to be replicated in ACP workforces at other NHS trusts, as previously concluded by Evans et al (2021) and Fogerill et al (2022).
Evans et al (2021) completed a scoping review to comprehensively map the evidence of ACP roles in the UK and highlight various implementation challenges. The study concluded that there is very little UK or international evidence related to the impact of ACP in terms of the research or education pillars, and limited amounts of evidence that evaluate activity away from the clinical pillar of ACP.
Initiating and running an online journal club is a low-cost, but effective, intervention. From this early innovation review, common pitfalls have been uncovered, but so have the interventions required to combat this.
The platform of this journal club allows for this to be expanded regionally to other ACPs to improve confidence within accessing research and reignite an interest within the research pillar. ACPs are the static workforce within a department and key to effective change implementation (Mann et al, 2023). Engaging more ACPs in research in a nurturing environment will encourage growth and expansion of the research pillar, therefore, leading to greater patient care through evidence-based interventions and improvements (Evans et al, 2021).
Conclusion
The ACP-lead journal club has increased ACP participation in research and is creating a culture of change and improved collaboration between clinical practice and the current evidence base. The idea of a journal club can seem archaic and outdated; however, times have changed and so have journal club formats. Journal clubs with a didactic format run the risk of attendees becoming passive listeners.
Therefore, alteration of the arrangement using a peer-learning approach increases engagement and confidence of the learner. The innovation described previously has uncovered common themes and barriers to accessing research engagement, which are likely to be echoed nationally and across multiple professions. The potential of online journal clubs are vast and expansion to regional or national clubs to address the issues discussed previously could further increase active engagement within research and inspire innovation.
KEY POINTS
- Research and critical appraisal are often thought of as inaccessible, difficult and intimidating
- A peer-based journal club with focus on the approach to critique, rather than the content, increases the confidence of the learner
- Traditional style and speciality-based journal clubs can be ineffectual in modern day healthcare settings
- The use of an online platform has increased participation and accessibility to research within the ACP community, with the aim being to expand nationally across multiple professions.
CPD / Reflective Questions
- Do you feel locally or as an individual that there is a negative attitude towards research participation? Why might this be?
- Could the contents of this article inform a change of practice for you? For example, joining a local journal club or starting your own online journal club?
- Do you feel there would be a difference in your own behaviours/interactions with a non-expert facilitator compared to an expert facilitator, as outlined in this article?
- Consider your own thoughts and feelings regarding being asked to present at a journal club; what aspects do you think would improve your confidence in doing this?


